Over one third of all U.S. health care payments are already flowing through alternative payment models — Where does your organization stand?
The Health Care Payment Learning and Action Network (HCPLAN) was launched in 2015 to accelerate the health care system’s transition to accountable care by combining the innovation, power, and reach of the private and public sectors. By sharing information about successful models and encouraging private entities to share their best practices, the HCPLAN works to reduce barriers and accelerate adoption of APMs. Learn more about our mission, vision and goals.
The HCPLAN is measuring nationwide progress toward APM adoption and accountable care to help build a more effective health care system. Health plans play a critical role in this process, as described below.
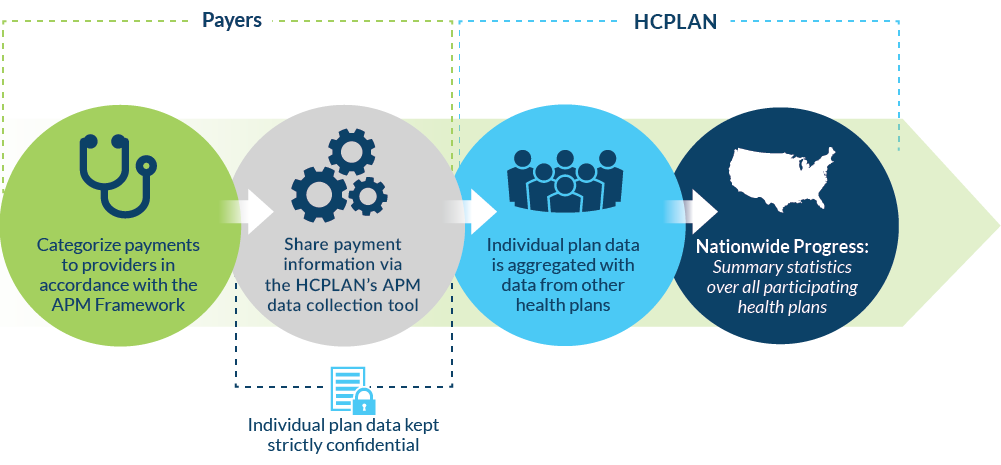
Each year the HCPLAN recruits health plans and other payers (e.g., state Medicaid agencies) in the Spring and releases results in the Fall. By using common definitions of alternative payments from the HCPLAN’s APM Framework, health plans across the country can contribute to and learn from our collective understanding of progress toward accountable care.
The HCPLAN is currently recruiting! Contact us to learn more about how you can get involved.
When reporting 2023 data in the 2024 Measurement Effort, participating payers will report total in- and out-of-network health care spending paid to providers through each of the categories and subcategories in 2023 or the most recent 12 months in the commercial, Medicaid and Medicare Advantage markets. For reporting purposes, individual payer data will be aggregated with data from other payers. Individual payer data will be kept strictly confidential. It will not be shared with other participants or parties outside of the HCPLAN data collection team.
More detailed information and helpful
resources on the HCPLAN Measurement Effort:
- 2024 APM Methodology Overview
- Frequently Asked Questions
- 2024 APM National Data Collection Metrics PDF
- 2024 APM National Data Collection Metrics Excel
- 2024 HCPLAN National Data Collection Survey
- Guidance for Measuring Covered Lives in
Accountable Care APM Arrangements - Refreshed APM Framework White Paper
- 2024 HCPLAN National Data Collection Training Webinar
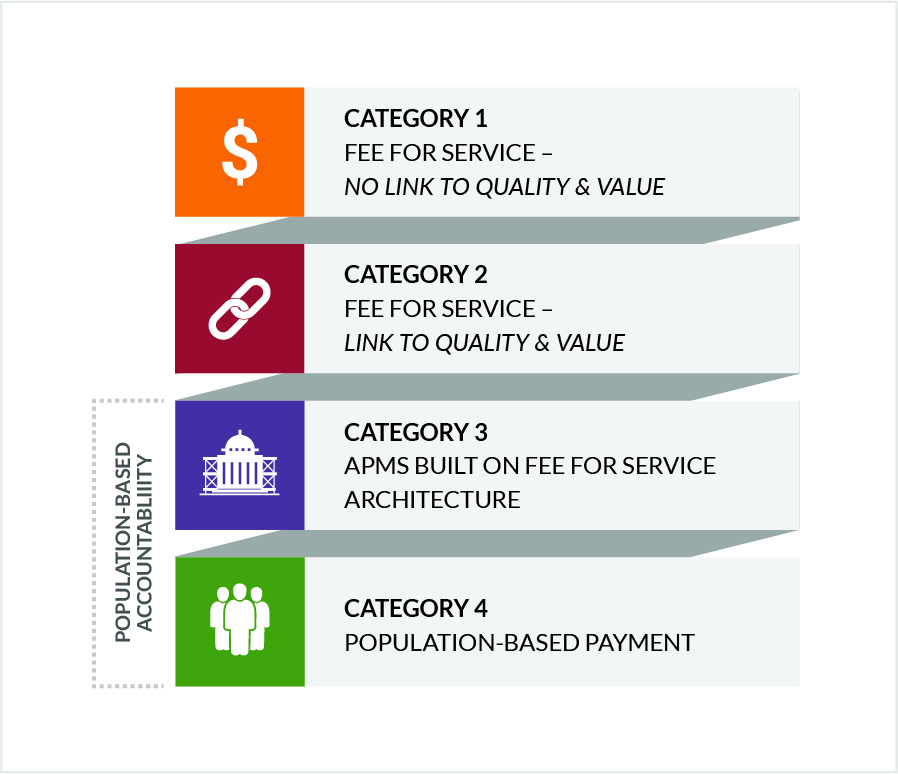
The HCPLAN’s APM Framework provides standardized definitions and categories of APMs. The HCPLAN published the original APM Framework in January of 2016 and refreshed it in 2017. The HCPLAN will continue to use the category definitions from the refreshed APM Framework to measure APMs, using similar metrics and methodology as were used in 2023.
To see the latest APM results, click here.
HCPLAN has adopted this uniform accountable care definition for the industry:
“Accountable Care” centers on the patient and aligns their care team to support shared decision-making and help realize the best achievable health outcomes for all through equitable, comprehensive, high quality, affordable, longitudinal care.
This definition was developed by the Accountable Care Action Collaborative (ACAC), which led several rounds of iteration and solicited written public input on it from 2022 HCPLAN Town Hall participants.
For the purposes of the annual HCPLAN measurement effort, lives in accountable care arrangements must include two elements: 1) the care is longitudinal with a duration of at least six months or longer; and 2) the payment model incorporates accountability for total cost of care (TCOC) for attributed patients.
To see the latest results of lives in accountable care arrangements, click here.
OMB Control Number: 0938-1297














 Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models.
Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models. Mr. James Sinkoff is the Deputy Executive Officer and Chief Financial Officer for Sun River Health (formerly known as Hudson River HealthCare), and the Chief Executive Officer of Solutions 4 Community Health (S4CH); an MSO serving FQHCs and private physician practices.
Mr. James Sinkoff is the Deputy Executive Officer and Chief Financial Officer for Sun River Health (formerly known as Hudson River HealthCare), and the Chief Executive Officer of Solutions 4 Community Health (S4CH); an MSO serving FQHCs and private physician practices. Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System.
Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System. Dr. Brandon G. Wilson, DrPH, MHA (he, him, his) joined Community Catalyst as the Director of the Center for Consumer Engagement in Health Innovation, where he leads the Center in bringing the community’s experience to the forefront of health systems transformation and health reform efforts, in order to deliver better care, better value and better health for every community, particularly vulnerable and historically underserved populations. The Center works directly with community advocates around the country to increase the skills and power they have to establish an effective voice at all levels of the health care system. The Center collaborates with innovative health plans, hospitals and providers to incorporate communities and their lived experience into the design of systems of care. The Center also works with state and federal policymakers to spur change that makes the health system more responsive to communities. And it provides consulting services to health plans, provider groups and other health care organizations to help them create meaningful structures for engagement with their communities.
Dr. Brandon G. Wilson, DrPH, MHA (he, him, his) joined Community Catalyst as the Director of the Center for Consumer Engagement in Health Innovation, where he leads the Center in bringing the community’s experience to the forefront of health systems transformation and health reform efforts, in order to deliver better care, better value and better health for every community, particularly vulnerable and historically underserved populations. The Center works directly with community advocates around the country to increase the skills and power they have to establish an effective voice at all levels of the health care system. The Center collaborates with innovative health plans, hospitals and providers to incorporate communities and their lived experience into the design of systems of care. The Center also works with state and federal policymakers to spur change that makes the health system more responsive to communities. And it provides consulting services to health plans, provider groups and other health care organizations to help them create meaningful structures for engagement with their communities. Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.
Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.


 Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.
Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.








