Colorado Innovations, The Commercial ACO Perspective
- September 21, 2017
- Posted by: Health Care Payment Learning & Action Network
- Category: Blog

Colorado provides a notable example of public and private collaboration, with lessons learned over the past five years that may help other regions accelerate their progress in payment reform. With regional data sharing and coordination as key levers in enabling the transformation, the state has learned the impact of payer commitment and alignment in an accountable care organization model.
Payer Commitment and Alignment
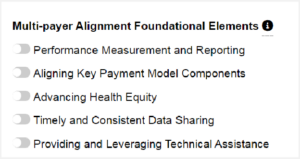
Public and private payers have voluntarily developed a Multi-Payer Collaborative (Collaborative) to support and expand broad-based accountable, whole-person, patient-centered care transformation, starting with the Comprehensive Primary Care initiative (CPC Classic) in 2012, continuing with the State Innovation Model grant in 2015, and also including CPC+ which started in 2017. The public sector has also been involved in payment transformation in Colorado. Eight payers, including Medicaid and Medicare, committed to work collaboratively and to provide resources to transform the way primary care is delivered across the state. Communication support and expert facilitation has built trust among stakeholders to maintain the Collaborative’s forward momentum. The Collaborative’s vision for success is a shared commitment to increased system accountability, improved health outcomes and experiences for patients and providers, decreased total cost of care, and continuous improvement and diffusion of innovative and successful strategies.
The Collaborative meets monthly to work on organizational alignment, consistency, and coordinated efforts among payers in support of practice transformation and improved patient outcomes. Organizational alignment is critical to help practices successfully transform measurement, payments, and practice goals. One of the Collaborative’s promising practices and a key to success has been its action of partnering with a core group of physician leaders to identify an aggregated multi-payer data solution for the state. Practices have found multi-payer data aggregation helpful in selecting targets for quality improvement and cost containment activities.
While each payer is using its own payment model to support primary care transformation goals, each payer committed to eventually align payment systems with either a Category 3 (APMs built on a FFS architecture) or a Category 4 model of the Health Care Payment and Learning Action Network’s APM Framework. Thus, these payers will eventually include in their payment systems shared savings opportunities or incentive payments based on performance and/or outcomes linked to quality.
Successes and Challenges of the Accountable Care Organization Model
The Collaborative builds on the payment reform and practice transformation support work payers are already doing and helps align outcome measures and clinical quality measures used by practices to influence healthcare quality, utilization, and costs. For example, in Colorado Medicaid, this work is aligned with the successful Accountable Care Collaborative that has improved health outcomes and lowered overall costs.
The commercial ACO landscape in Colorado has evolved rapidly over the past five years, and now encompasses four of the major national payers: Aetna, Anthem, Cigna, and United Healthcare all developed programs with sophisticated infrastructures. Colorado has a well-functioning cloud-based information exchange which has facilitated the development of these approaches and advanced the goals of improved health, smarter spending, and quality care via the following attributes:
- Patients are engaged within an ACO system of care that is better coordinated, resulting in measurably improved quality and efficiency of care.
- Case management is enhanced with improved linkage between the case management services of the payers and physician organizations, along with markedly better data sharing between the entities, allowing for improved care coordination.
- Population-based health predictive analytics are applied to these patient populations, allowing for risk stratification and prospective case management.
- Claims analyses can be shared from the payer to the physician organizations, allowing the selection of providers to the most efficient sites of service.
Simultaneously, there are constraints within the payers which limit the potential benefits of the ACO model. These restrictions include:
- Within payer organizations, there continues to be a dynamic tension between sales and marketing and medical management, with the former promoting open access to broad panels and the latter working to define the optimal physician/hospital network based upon quality and efficiency parameters. It is a flawed assumption to think patients will reliably choose high quality/efficiency providers in an open access provider panel. ACO’s should improve both quality and efficiency by choosing a narrower, high functioning provider panel.
- Many payers are unwilling to share complete claims information, which significantly limits the ability of the physician organization to stratify providers based upon optimal efficiency.
- Reimbursement methodologies are tied to the FFS/gainshare model of care delivery, which creates challenges for evolving to population health/capitation methodologies.
In addition to these limitations, Colorado, along with some other states, is further hampered by “incident to” legislation which forces the payers to pay billed charges to entities when they are brought into a case by another provider. Common scenarios include neuromonitoring, anesthesia, surgical assistants, etc. Some of these charges are significant and pose challenges for the ACO to stay within budget.
These constraints need to be addressed in order to continue realizing improvements in quality and efficiency; otherwise, the gains will attenuate over time. To date, however, the positives have outweighed the negatives, and the forces thus applied to the provider community are aligning care in the correct direction, moving the needle on both quality and efficiency. The Colorado experience illustrates how successful reform in payment and delivery rests on physicians and payers aligning to work together.
Authors’ Note
Ken Cohen MD, FACP, Chief Medical Officer, New West Physicians
Judy Zerzan, MD, MPH, Chief Medical Officer / Office Director, Colorado Department of Health Care Policy & Financing.
















 Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models.
Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models. Mr. James Sinkoff is the Deputy Executive Officer and Chief Financial Officer for Sun River Health (formerly known as Hudson River HealthCare), and the Chief Executive Officer of Solutions 4 Community Health (S4CH); an MSO serving FQHCs and private physician practices.
Mr. James Sinkoff is the Deputy Executive Officer and Chief Financial Officer for Sun River Health (formerly known as Hudson River HealthCare), and the Chief Executive Officer of Solutions 4 Community Health (S4CH); an MSO serving FQHCs and private physician practices. Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System.
Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System. Dr. Brandon G. Wilson, DrPH, MHA (he, him, his) joined Community Catalyst as the Director of the Center for Consumer Engagement in Health Innovation, where he leads the Center in bringing the community’s experience to the forefront of health systems transformation and health reform efforts, in order to deliver better care, better value and better health for every community, particularly vulnerable and historically underserved populations. The Center works directly with community advocates around the country to increase the skills and power they have to establish an effective voice at all levels of the health care system. The Center collaborates with innovative health plans, hospitals and providers to incorporate communities and their lived experience into the design of systems of care. The Center also works with state and federal policymakers to spur change that makes the health system more responsive to communities. And it provides consulting services to health plans, provider groups and other health care organizations to help them create meaningful structures for engagement with their communities.
Dr. Brandon G. Wilson, DrPH, MHA (he, him, his) joined Community Catalyst as the Director of the Center for Consumer Engagement in Health Innovation, where he leads the Center in bringing the community’s experience to the forefront of health systems transformation and health reform efforts, in order to deliver better care, better value and better health for every community, particularly vulnerable and historically underserved populations. The Center works directly with community advocates around the country to increase the skills and power they have to establish an effective voice at all levels of the health care system. The Center collaborates with innovative health plans, hospitals and providers to incorporate communities and their lived experience into the design of systems of care. The Center also works with state and federal policymakers to spur change that makes the health system more responsive to communities. And it provides consulting services to health plans, provider groups and other health care organizations to help them create meaningful structures for engagement with their communities. Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.
Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.


 Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.
Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.








