2024 Q2 Newsletter | July 2024
- July 29, 2024
- Posted by: Health Care Payment Learning & Action Network
- Categories: eNewsletter, Uncategorized
Register today for the 2024 Health Care Payment Learning & Action Network (HCPLAN) Summit on November 14, 2024 at the Baltimore Convention Center!
Attend the 2024 Summit to participate in live sessions focused on health equity, multi-payer alignment, improved patient and family experience, and more! Hear directly from state leaders, industry experts, and federal government officials as they share useful strategies, best practices, real-life experiences, and updates from the field. And be the first to see the results of the 2024 Measurement Effort, the most comprehensive snapshot available for measuring progress on payment reform nationwide!
Registration is now LIVE! Sign up for free by visiting www.hcplansummit.org.
Some sessions will be available via livestream, but we hope to see you there in person!
Investing in Community –
HEAT Partnership Spotlight

The Southern Alabama Regional Council on Aging (SARCOA) is the community-based organization (CBO) featured in this quarter’s HCPLAN Health Equity Advisory Team (HEAT) partnership spotlight! Read on to learn more about their exciting work, with insights from SARCOA Director of Home and Community Services Joseph D. Strickland and Executive Director Kimberly Falkner.
Q: Tell us more about SARCOA’s work and the community it serves.
A: SARCOA is an Area Agency on Aging serving the seniors of the wiregrass region of southeast Alabama. We are dedicated to enhancing our seniors’ independence and quality of life through planning, coordinating, and developing community services. SARCOA focuses on delivering high-quality, caring, and trustworthy services that embrace innovation and excellence.
Q: In what ways does SARCOA’s work align with the HEAT CBO Guidance Document and its recommendations?
A: As we participated in the HCPLAN process and reviewed the Guidance Document’s list of cross-sectoral financing opportunities for social needs services, we reflected on our own approach. We determined that it was necessary to reduce utilization of section 1115 and 1915 Medicaid waivers by improving health awareness, compliance with medical guidance, and understanding of alternative value-based payment solutions. Collaborating with federal, state, local, and health plan partners has shown significant return on investment and is vital, especially with current funding uncertainties. The HEAT process has strengthened our mission and energized our leadership.
Q: How have the HEAT CBO recommendations influenced your engagement with alternative payment models (APMs) and payers?
A: SARCOA continues to strengthen relationships with stakeholders and purchasers of our services, leveraging our experience and resources. Our leadership team, with nearly 100 years of combined experience, strategically selects projects aligning with our mission. Developing relationships with peer CBO HEAT professionals has expanded our reach and strengthened our business model.
Q: What are your organization’s future plans to strengthen CBO-APM partnerships and improve health equity?
A: SARCOA aims to remain a respected and valued resource for seniors seeking to stay independent. We plan to leverage our experience, resources, and relationships to ensure the individuals we serve are healthy, active, and able to remain independent within their communities.
Spotlight on Action

At the April meeting of the Accountable Care Action Collaborative (ACAC), Chris Botts and his team from the American Medical Association (AMA) provided an overview of the collaborative efforts of the AMA, AHIP, and the National Association of Accountable Care Organizations (NAACOS). Botts highlighted their release of two playbooks—one focused on data sharing and the other on payment arrangements—which together deliver 90 best practices for establishing value-based care (VBC) arrangements. Botts emphasized that these best practices are critical for creating pathways towards VBC, balancing alignment and flexibility, and ensuring transparency across various domains. Learn more about these playbooks by following the links provided:
- The Future of Sustainable Value-Based Care and Payment: Voluntary Best Practices to Advance Data Sharing
- Creating a Sustainable Future for Value-Based Care: A Playbook of Voluntary Best Practices for VBC Payment Arrangements
Botts also emphasized the importance of integrating digital health into VBC. As part of the AMA’s independent Future of Health initiative, the AMA plans to develop case studies illustrating successful implementation of virtual VBC arrangements. These 10-page case studies will provide detailed examples of best practices in action, measuring their success in diverse market environments and providing actionable insights to guide other organizations looking to implement them.
Additionally, Botts touched on the need for continued evaluation and testing of these best practices and acknowledged the ongoing financial investment the associated data collection requires. He emphasized that these efforts are ultimately intended to support providers in delivering high-quality care while reducing administrative burden, making health care delivery overall more efficient and fulfilling for providers.
HCPLAN News
Recap: Addressing Climate Change to Accelerate Value-Based Care Webinar
On May 8, 2024, HCPLAN co-hosted the “Addressing Climate Change to Accelerate Value-Based Care” webinar along with the U.S. Department of Health and Human Services (HHS) Office of Climate Change and Health Equity (OCCHE). OCCHE aims to prepare health care organizations for climate challenges and reduce their emissions through initiatives like those funded by the Inflation Reduction Act. This webinar brought together key figures from a variety of health care organizations to focus on the intersection of climate change and health equity.
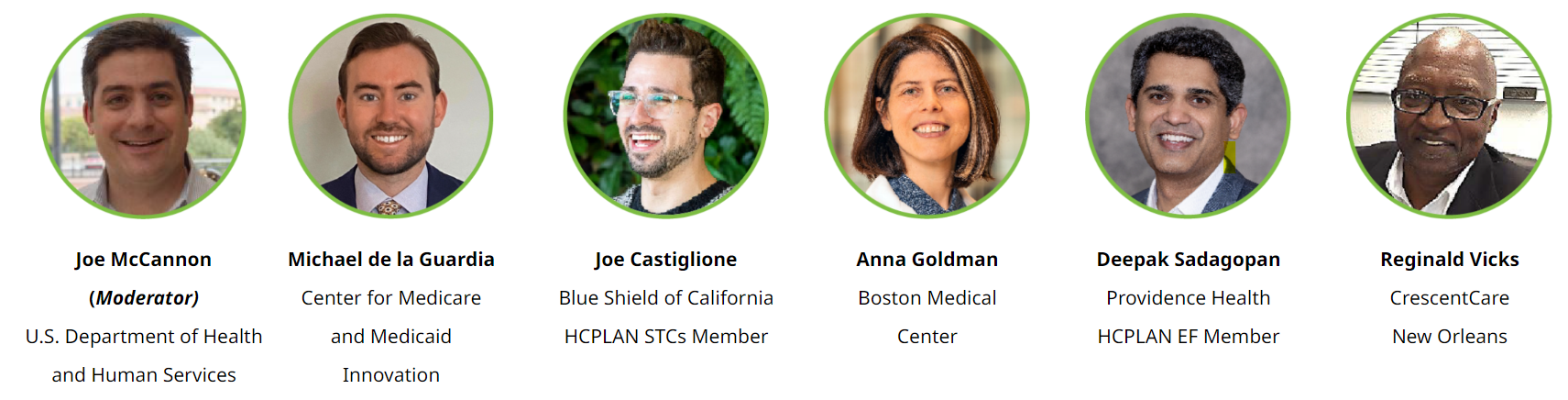
Panelists Anna Goldman, Deepak Sadagopan, Reginald Vicks, and Joe Castiglione shared their organizations’ strategies for integrating climate resilience into health care. As frequently mentioned by these speakers, certain populations experience a disproportionately greater share of the effects of climate change, due to discrimination and underinvestment in their communities. Initiatives such as Boston Medical Center’s Clean Power Prescription program and CrescentCare’s Community Lighthouse Project aim to address these disparities. The speakers also explained how upstream health investments and aligning climate initiatives with financial recovery can reduce economic barriers to health care access.
Additionally, speakers listed activities, such as coordinating community resources and fostering dialogue among payers, providers, CBOs, and employers, that can help improve mobilization and minimize disruptions in patient care. Michael de la Guardia of the Center for Medicare and Medicaid Innovation (CMMI) discussed the Transforming Episode Accountability Model (TEAM), a new episode-based payment model that includes a voluntary Decarbonization and Resilience Initiative, intended for launch in 2026. The initiative aims to take on the health impacts of greenhouse gas emissions by creating a voluntary reporting system and providing technical assistance/learning support for hospitals undertaking decarbonization activities.
For the full conversation about improving health outcomes while addressing climate change, check out the webinar recording.
New Executive Forum Member: Dr. Sree Chaguturu

Welcome to our newest member, Sree Chaguturu, M.D., executive vice president and chief medical officer of CVS Health! The mission of CVS Health is to deliver affordable, high-quality, customer-centered care that improves the health and well-being of the people they serve. Dr. Chaguturu’s work focuses on assuring clinical quality standards, increasing access to care, improving patient outcomes, and keeping health care costs affordable across the CVS Health enterprise. He joins the rest of the Executive Forum in identifying tools and strategies that can help the HCPLAN and its partners accelerate the adoption of alternative payment models and accountable care and shape the transformation of health care delivery.
New Accountable Care Action Collaborative (ACAC) Member: National Association of Chain Drug Stores (NACDS)

The National Association of Chain Drug Stores (NACDS) recently joined the HCPLAN’s ACAC. NACDS represents traditional drugstores along with supermarkets and mass merchants that have pharmacies. Its mission is to foster the growth of the chain community pharmacy industry and promote the role of chain community pharmacies as trusted neighborhood providers of health care services and products. NACDS joins a long list of dedicated ACAC members working together to transform the accountable care landscape beyond payment reform.
The North Carolina State Transformation Collaborative outlined action items to enhance VBC and quality measurement during a May webinar. Their recommendations focused on improving data integration, patient engagement, and care coordination to foster better health outcomes and system efficiency. Read more.
The American Medical Association, an Accountable Care Action Collaborative member, shared seven key strategies for success in value-based care payment arrangements on its website. From patient attribution to financial risk and benchmarking, their guide covers the topics essential for all health care professionals transitioning to value-based models. Learn more.
Prioritization of individual social-needs screening in health care may strip energy, attention, and resources from the goal of advancing equity in patient experience and clinical outcomes. Dive into the insights of Health Equity Advisory Team Co-Chair Dr. Marshall Chin in his New England Journal of Medicine perspective piece “Keep Your Eyes on the Prize – Focusing on Health Care Equity,” co-authored with Dr. Alicia Fernandez.
Our Vision
Improved and equitable health outcomes, resulting in overall lower total cost of care.
Our Mission
The HCPLAN will advance multi-stakeholder payment reforms to enable coordinated health care that achieves better health, equity, and affordability.
Our Goal Statement
Accelerate the percentage of U.S. health care payments tied to quality and value in each market segment through the adoption of two-sided risk alternative payment models (Categories 3B and 4 of the HCPLAN APM Framework).


















 Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models.
Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models. Mr. James Sinkoff is the Deputy Executive Officer and Chief Financial Officer for Sun River Health (formerly known as Hudson River HealthCare), and the Chief Executive Officer of Solutions 4 Community Health (S4CH); an MSO serving FQHCs and private physician practices.
Mr. James Sinkoff is the Deputy Executive Officer and Chief Financial Officer for Sun River Health (formerly known as Hudson River HealthCare), and the Chief Executive Officer of Solutions 4 Community Health (S4CH); an MSO serving FQHCs and private physician practices. Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System.
Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System. Dr. Brandon G. Wilson, DrPH, MHA (he, him, his) joined Community Catalyst as the Director of the Center for Consumer Engagement in Health Innovation, where he leads the Center in bringing the community’s experience to the forefront of health systems transformation and health reform efforts, in order to deliver better care, better value and better health for every community, particularly vulnerable and historically underserved populations. The Center works directly with community advocates around the country to increase the skills and power they have to establish an effective voice at all levels of the health care system. The Center collaborates with innovative health plans, hospitals and providers to incorporate communities and their lived experience into the design of systems of care. The Center also works with state and federal policymakers to spur change that makes the health system more responsive to communities. And it provides consulting services to health plans, provider groups and other health care organizations to help them create meaningful structures for engagement with their communities.
Dr. Brandon G. Wilson, DrPH, MHA (he, him, his) joined Community Catalyst as the Director of the Center for Consumer Engagement in Health Innovation, where he leads the Center in bringing the community’s experience to the forefront of health systems transformation and health reform efforts, in order to deliver better care, better value and better health for every community, particularly vulnerable and historically underserved populations. The Center works directly with community advocates around the country to increase the skills and power they have to establish an effective voice at all levels of the health care system. The Center collaborates with innovative health plans, hospitals and providers to incorporate communities and their lived experience into the design of systems of care. The Center also works with state and federal policymakers to spur change that makes the health system more responsive to communities. And it provides consulting services to health plans, provider groups and other health care organizations to help them create meaningful structures for engagement with their communities. Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.
Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.


 Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.
Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.









