2021 Summit Update | February 8, 2022

2021 LAN Summit Summary
Over 1,400 LAN stakeholders came together during the virtual 2021 LAN Summit to discuss the most pressing issues surrounding the payment, delivery, and quality of care in the United States. The LAN’s new work at the state level through their State Transformation Collaboratives (STCs) and the Accountable Care Action Collaborative, vision for greater health equity, and the shortcomings in care exposed by the COVID-19 pandemic, were several top-of-mind issues that were discussed in detail during the Summit.
How can payers, purchasers, and providers deliver better care to patients? How can we overcome disparities in care for different populations? Can we correct the system flaws that COVID exposed? These and other questions were discussed throughout the Summit. State-level alternative payment models (APMs) emerged as one of the best ways to remedy what ails our struggling health care system. Transitioning from a fee-for-service (FFS) model to focus on the whole person and valuing outcomes more than procedures will remediate many of the challenges in equitable care delivery. According to LAN CEO Forum Co-Chair and CEO of Intermountain Healthcare Dr. Marc Harrison, practices with APMs have fared much better during the pandemic than their FFS counterparts. According to Dr. Harrison, FFS providers have “had their lunch eaten” during the pandemic—exposing not only flaws in how care is delivered but also in the type of care FFS allows.
“The LAN has been a source of strength and collaboration for many of us while we make health care more equitable and affordable,” Care Transformation Co-Chair Emily Brower said before encouraging attendees to share LAN resources with their networks because they are “the go-to resource for the why, where and how of improving care.”
Throughout the Summit, some of healthcare’s biggest innovators and thought leaders articulated why this is the time to act. Attendees heard the potential and promise that value-based payment models can unleash—providing better and more equitable care at a lower overall cost.
This year’s Summit also had a sense of urgency. “The time is now” was a common refrain heard from the likes of CMS Administrator Chiquita Brooks-LaSure, Health Equity Advisory Team (HEAT) Co-Chair Karen Dale, Families USA Executive Director Frederick Isasi, and Center for Medicare and Medicaid Innovation (CMMI) Director Elizabeth Fowler.
Given the sense of urgency and this unique opportunity in time, several new LAN initiatives were announced, including the LAN 3.0 framework which moves the organization to a more action-oriented role. State Transformation Collaboratives (STCs)and the Accountable Care Action Collaborative (AC AC) will add diverse voices and creative solutions to designing APMs that meet the needs of local populations.
The release of the last two years of APM measurement data proves that more needs to be done to further the use of local APMs. Federal payers are eager participants in this new state-level strategy. Strong support was reiterated by CMS Administrator Chiquita Brooks-LaSure, CMMI Director Elizabeth Fowler, Center for Medicare and CHIP Services Director Daniel Tsai, and Center for Medicare Director Dr. Meena Seshamani—all of whom support the LAN’s pivot to a more active role.
Medicaid is “committed to pushing patient-centered care forward,” said Director of Medicaid and CHIP Services Daniel Tsai. “We are very focused on how to measure disparities, figure out how to partner together on innovations and investments…and doing everything possible to advance value-based care in Medicaid…CMCS and CMS will be leaning into the LAN in years to come.”
“Payers and providers are both really focusing on equity…Now is the time to drive towards more equitable, value-based care.”
– LAN Care Transformation Co-Chair Dr. Will Shrank.
To lead the change needed in healthcare, this year’s attendees heard more about the HEAT’s first publication, Advancing Health Equity through APMs: Guidance for Equity-Centered Design and Implementation. It offers guidelines and best practices for incorporating equity into APM design and ensures person-centered care includes all people, regardless of age, race, zip code, or social determinants of health.
Stakeholders heard updates about APMs, including design best practices, strategies, and real-world examples of successes and barriers to implementation from the state and regional perspective. Additionally, attendees heard directly about the LAN’s new, innovative initiatives, including perspectives from leaders in the first four states—Arkansas, California, Colorado, and North Carolina—to serve as the inaugural class for the LAN’s State Transformation Collaboratives.
“Now is the time,” CEO Forum Co-Chair Dr. Mark McClellan reiterated as he brought the 2021 LAN Summit to a close. The hard work of seeing APMs implemented and better, more equitable care as the desired outcome must begin in earnest. You can contribute to this cause by becoming more involved with the LAN, helping shape its progress and its future, and being a catalyst for lasting, positive change to the nation’s health care system.
Thank you to everyone who participated in this year’s Summit and helped make it a great success. Below is a more in-depth look at the new initiatives and the data the LAN unveiled during the 2021 Summit.
Stay involved and seize this moment! Check out the entire Summit on the LAN Summit’s website and find ways you can get involved in this challenging and fulfilling work.
LAN 3.0: Taking Action and Focusing on Health Equity
CEO Forum Co-Chair Dr. Mark McClellan addressed the Summit and stated that the LAN was going to “focus squarely on the goals that APMs will achieve,” while fee-for-service payment models continue to keep “too many people locked out of the care that they need and locks providers out of payment models that let them meet patients where they are.”
In response to the COVID pandemic, Dr. McClellan stated that both the need and the evidence for APM’s advantages were glaringly clear. With APMs comes the promise of more equitable care. The guiding principle for the LAN and its new role under LAN 3.0 as a facilitator rather than just an advocate for payment reform is that the “North Star [of payment reform] is still better care at lower costs.”
Transitioning to a person-centered and value-based system of healthcare will be a challenge, said CMS Administrator Chiquita Brooks-LaSure in support of LAN 3.0. It is, however, a challenge that both CMS and the LAN are ready—and readily-equipped—to face. Under CMS leadership and a newly-empowered LAN, the work of creating a more just and equitable healthcare system is underway.
The ongoing pandemic was a looming presence throughout the 2021 LAN Summit. COVID is, in part, one of the catalysts for the evolution to a more activist LAN because the virus “has profoundly exposed that our healthcare system does not produce equitable outcomes,” according to Dr. McClellan. The silver lining of what COVID exposed is that “we now have opportunity to address [health equity] with momentum on our side.”
“We can, must, and will do more to shift away from fee-for-service towards value models…
[the] failings of our health system was laid bare by COVID-19.”
– CMS Administrator Chiquita Brooks-LaSure
Stay involved, and seize this moment! Check out the entire Summit on the LAN Summit’s website, and find ways you can get involved in this challenging and fulfilling work.
2019 and 2020 APM Measurement Results
The LAN’s much-anticipated measurement data—covering both 2019 and 2020—was analyzed and discussed by a panel of healthcare leaders including: Dr. Will Shrank, LAN Care Transformation Forum Co-Chair and Humana CMO, Dr. Purva Rawal, CMMI Chief Strategy Officer, Dr. Andrea Gelzer, Senior Vice President of Medical Affairs at AmeriHealth Caritas, and Dr. John Bulger, Chief Medical Officer at Geisinger Health Plan. The panel was moderated by Andréa Caballero, Program Director for Catalyst for Payment Reform. Panelists urged attendees to use this data and to seize this unique moment to transform healthcare into a more equitable system that is outcomes-based and patient-centered.
During the discussion, panelists took attendees on a “tour of what we’ve learned over the past two years with APM adoption,” according to moderator Andréa Caballero, who shared some of the high-level findings of the past two years of APM measurement results.
The full results of the measurement data are available on the LAN website.
“Part of the [CMMI strategy] refresh was developing a new vision: to achieve equitable outcomes
through high-quality, affordable, and patient-centered care.”
– CMMI Chief Strategy Officer Purva Rawal
Dr. Will Shrank stated that the “level of partnership between payer and provider has only grown…The pandemic accelerated that openness to move towards risk arrangements because the pandemic was overwhelming for many provider organizations.” Dr. Shrank elaborated by saying that providers using value-based payment models fared better than traditional FFS providers and that now is the time to transition more providers to APMs.
Equity, too, was at the forefront of the conversation. Dr. Shrank said, “As more and more light has been shone on the issues of inequities and disparities in healthcare delivery, it’s awesome to see the level of engagement nationally of plans and providers around really focusing on the issue of equity and really bringing that to the forefront in terms of both measurement and how we’re ultimately going to reward and align payment for providers.”
Panelists agreed that the measurement data for APM adoption is a lagging indicator. Stressing the need for action now, there was broad agreement that the true impact that COVID has had on the transition to value-based care wouldn’t be seen until next year and perhaps the following year.
Stay involved and seize this moment! Check out the entire Summit on the LAN Summit’s website and find ways you can get involved in this challenging and fulfilling work.
The HEAT’s APM Guidance Document
The Health Equity Advisory Team (HEAT) launched its first publication—a guidance document entitled, Advancing Health Equity through APMs—during the 2021 LAN Summit. The guidance document advances the role of health equity at the center of healthcare.
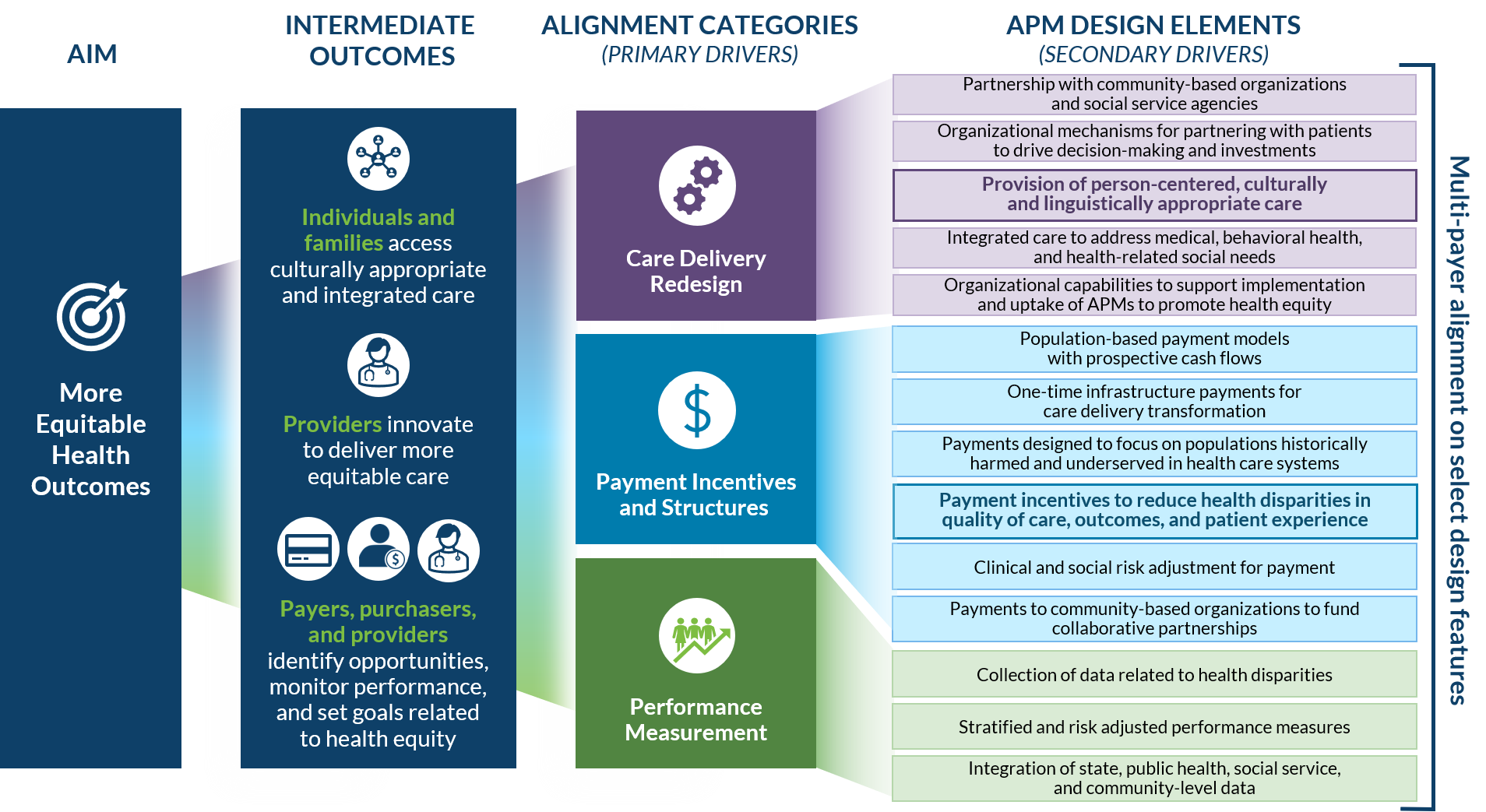
Dr. Chin discussed the HEAT’s Theory of Change, which illustrates how alternative payment models (APMs) can be structured to advance health equity during a session that focused on the guidance document.
“The goal of the HEAT…is to be patient-centered…to help alternative payment models make needed care
more accessible, drive better outcomes and reduce health disparities.”
– Dr. Marshall Chin, HEAT Co-Chair
The resources contained in the guidance document focus on two critical design elements: Care Delivery Redesign and Payment and Incentives Structures. The resources provide metrics, methodologies, measurement sets, technical definitions, and illustrations to support stakeholders, including under-resourced providers and community health workforces, as they work to mitigate social determinants of health and barriers to equitable care.
The full guidance document is available on the LAN’s website to download and share with stakeholders in your community.
Stay involved, and seize this moment! Check out the entire Summit on the LAN Summit’s website, and find ways you can get involved in this challenging and fulfilling work. Additionally, you can click here to sign up for the LAN Newsletter for up-to-date news on the HEAT and LAN’s mission for equitable value-based APM design.
State Transformation Collaboratives and Accountable Care Action Collaborative
The LAN’s new initiatives, the State Transformation Collaboratives (STC) and the Accountable Care Action Collaborative (AC AC), will help to promulgate the adoption, transition, and transformation from fee-for-service to value-based payment models on the local, regional, and state level. Four states, Arkansas, California, Colorado, and North Carolina, were announced as the first pilot states to participate in the STC initiative.
The STCs, which are comprised of payers, providers, health systems, purchasers, patient advocates, and community organizations, seek to continue to shift the economic drivers away from fee-for-service to a value-based, person-centered approach to health through Medicaid and Medicare collaboration and partnership.
During a related panel discussion, representatives from each of the pilot states and federal health expert Dr. Ellen-Marie Whelan, Chief Population Health Officer at the Center for Medicaid and CHIP Services (CMCS) Centers for Medicare and Medicaid Services (CMS), took a deeper dive into the new LAN STCs as well as some innovative practices currently underway at the state level in each location.
The panel, moderated by Families USA Executive Director Frederick Isasi, explored how APMs can be designed with equity, innovation, and a focus on the patient as priorities. Whole-person and preventive care as well as commitments to equity and value were cited often as both the primary benefits as well as the motivators to transition to APMs rather than continuing to rely on fee-for-service models.
“Arkansas is committed to building equity and to value-based payments,” Alicia Berkemeyer from Arkansas Blue Cross Blue Shield said. “COVID has exposed the need to transition to a system based on value rather than fee-for-service.”
The LAN’s collaboratives will help with the design and implementation of APMs on the state level. According to CMS Administrator Brooks-LaSure, the state-level pilot programs “will serve as test cases to transition to a more locally-focused approach” to APM adoption.
“The LAN must make the next bold step to transition from empowerment to enablement,” continued Administrator Brooks-LaSure, who also reiterated that “this work is exciting, challenging, and necessary.”
By working on the local level with local experts and organizations, STCs will help design APMs with the goal of addressing the needs of state populations through value-based care models that are tailored to their respective needs. The AC AC will contribute to the success of STCs by:
- Facilitating forums for sharing cross-state knowledge and information, including guidance, resources, and subject matter expertise
- Collecting and synthesizing data on cross-state efforts
- Scaling promising practices and learnings to the regional and/or national levels
“The LAN must make the next bold step to transition from empowerment to enablement.”
– CMS Administrator Chiquita Brooks-LaSure.
To find out more about the LAN’s newest initiatives, please review this infographic and refer back to the write-up on the Role of APMs in Health Equity session, or review the Summit resources on the LAN Summit’s website.
Stay involved, and seize this moment! Check out the entire Summit on the LAN Summit’s website and find ways you can get involved in this challenging and fulfilling work. Additionally, you can click here to sign up for the LAN Newsletter for up-to-date news on the HEAT and the LAN’s mission for equitable value-based APM design.
LAN in the News
Chiquita Brooks-LaSure, Elizabeth Fowler
Read: CMS Innovation Center Strategic Direction: Background on the CMS Innovation Center 2021 Strategy Refresh – Putting All Patients at the Center of Care• The CMS Innovation Center, having taken stock of lessons learned from its first decade and 50+ models, is charting a path for the next ten years of value-based care—one that will improve the health system for all patients.
LAN Co-Chair Dr. Marc Harrison
Read: Harvard Business Review: 5 Critical Priorities for the U.S. Health Care System• “Without a faster shift to value-based care, the cost of health care in the United States will continue to rise. That is not sustainable for both provider institutions and patients. For many Americans, health care is already unaffordable and difficult to access.”
Organization: Oak Street Health
Read: Oak Street Health Selected by AARP as the Only Primary Care Provider to Carry the AARP Name• “As we pursue our mission to rebuild healthcare as it should be, our selection by AARP will enable us to better reach the Medicare-eligible population,” said Mike Pykosz, Chief Executive Officer of Oak Street Health.
Executive Forum Member Dr. Jaewon Ryu
Read: Modern Healthcare’s Top Diversity Leaders in Healthcare – 2021• Dr. Ryu was recognized as one of the Top 25 Modern Healthcare Diversity Leaders.
Care Transformation Forum Member Dr. Griffin Myers
Listen: Race to Value Podcast: Value-Based Care: A Superior Technology to Create Trusting Relationships, with Dr. Griffin Myers• Dr. Myers shares the importance of segmenting a patient population within a payment model that is better aligned with care outcomes.
Our Vision
An American healthcare system that pays for value to the benefit of our patients and communities.
Our Mission
To accelerate the shift to value-based care in order to achieve better outcomes at lower cost.
Our Goal Statement
Accelerate the percentage of US healthcare payments tied to quality and value in each market segment through the adoption of two-sided risk alternative payment models.























 Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models.
Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models. Mr. James Sinkoff is the Deputy Executive Officer and Chief Financial Officer for Sun River Health (formerly known as Hudson River HealthCare), and the Chief Executive Officer of Solutions 4 Community Health (S4CH); an MSO serving FQHCs and private physician practices.
Mr. James Sinkoff is the Deputy Executive Officer and Chief Financial Officer for Sun River Health (formerly known as Hudson River HealthCare), and the Chief Executive Officer of Solutions 4 Community Health (S4CH); an MSO serving FQHCs and private physician practices. Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System.
Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System. Dr. Brandon G. Wilson, DrPH, MHA (he, him, his) joined Community Catalyst as the Director of the Center for Consumer Engagement in Health Innovation, where he leads the Center in bringing the community’s experience to the forefront of health systems transformation and health reform efforts, in order to deliver better care, better value and better health for every community, particularly vulnerable and historically underserved populations. The Center works directly with community advocates around the country to increase the skills and power they have to establish an effective voice at all levels of the health care system. The Center collaborates with innovative health plans, hospitals and providers to incorporate communities and their lived experience into the design of systems of care. The Center also works with state and federal policymakers to spur change that makes the health system more responsive to communities. And it provides consulting services to health plans, provider groups and other health care organizations to help them create meaningful structures for engagement with their communities.
Dr. Brandon G. Wilson, DrPH, MHA (he, him, his) joined Community Catalyst as the Director of the Center for Consumer Engagement in Health Innovation, where he leads the Center in bringing the community’s experience to the forefront of health systems transformation and health reform efforts, in order to deliver better care, better value and better health for every community, particularly vulnerable and historically underserved populations. The Center works directly with community advocates around the country to increase the skills and power they have to establish an effective voice at all levels of the health care system. The Center collaborates with innovative health plans, hospitals and providers to incorporate communities and their lived experience into the design of systems of care. The Center also works with state and federal policymakers to spur change that makes the health system more responsive to communities. And it provides consulting services to health plans, provider groups and other health care organizations to help them create meaningful structures for engagement with their communities. Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.
Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.


 Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.
Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.








