2021 Q1 Newsletter | April 12, 2021
- April 12, 2021
- Posted by: Health Care Payment Learning & Action Network
- Categories: eNewsletter, Uncategorized

LAN’s Healthcare Resiliency Work Featured at the CMS Quality Conference!
Recently, the LAN’s Executive Forum co-chairs led a session at the CMS Quality Conference – Health Care Payment Learning and Action Network Healthcare Resiliency Collaborative: Lessons from the PHE for Value-Based Payment. The session was held on March 2, 2021, and highlighted the work of the LAN’s Healthcare Resiliency Collaborative. The co-chairs discussed why the LAN chose to develop the Healthcare Resiliency Framework, its support by industry leaders based on shared goals, and the initiative’s focus on resilience. The co-chairs addressed short- and long-term actions that stakeholders can implement to move health care payment forward in value-based care. The session also stressed the need to capitalize on lessons learned during the COVID-19 pandemic. Providers whose practices focus on value-based payment appeared to fare better financially and were more equipped to respond to the needs of their respective patient populations. Dr. Harrison, Dr. Shrank, and Ms. Brower spoke individually about what their organizations did during the pandemic that tied to actions in the Healthcare Resiliency Framework.
Dr. Marc Harrison, CEO and President at Intermountain Healthcare, spoke about the ability to do “the right things” in meeting the needs of patients with a value-based payment structure that facilitates quick decisions and changes for the health and safety of patients. He also acknowledged that by working as a system his organization was able to keep critically ill patients in smaller facilities with access to quality care. Intermountain Healthcare also was able to do clinical trials across three states with the use of digital enrollment. 70 percent of its COVID patients participated in one trial or another. Dr. Harrison commented, “Lots of good things can be done when you are playing as a team.”
Ms. Emily Brower, Senior Vice President of Clinical Integration and Physician Services at Trinity Health, underscored that the pandemic re-energized her organization to commit to value-based care to ensure quality patient care and outcomes. Trinity Health found it had the capabilities within its population health teams to pivot and quickly respond to protect its populations around the impacts of COVID-19. Payment models that fall within the Category 4 LAN taxonomy sustained the organization and supported the deployment of technology to address the immediate needs of its patients. She expressed striving for that payment model and approach for more of Trinity Health’s patients.
Dr. Will Shrank, Chief Medical Officer at Humana, spoke about the opportunity provided by the shared commitment of the Healthcare Resiliency Framework as a launching pad for his organization to work on a common set of principles to best serve patients with contracted providers. Dr. Shrank also emphasized the need to promote equity. He commented that the pandemic “shines a bright light” on the varied experiences different populations face and that we must be intentional in how we measure equity to help reduce disparities. His organization is actively collaborating with other large organizations to tackle social determinants of health.
Following the presentation, the co-chairs responded to audience questions on a variety of topics, including: resiliency for providers operating in value-based payment arrangements during COVID-19; post-acute care’s role in the continuum of care; the role of telehealth in providing care to patients; Medicaid value-based payment models and impact on social determinants of health; as well as the need for coordination of care between primary care and specialty care providers as shown in bundled payment models.
Dr. Mark McClellan, Director at the Duke-Margolis Center for Health Policy, closed the session by referencing the LAN’s ongoing work in health equity. He noted that there will be opportunities for organizations to join this work with more details to follow in the upcoming months.
Stay tuned to hear more about the LAN’s next initiative that will build upon the work of the Healthcare Resiliency Collaborative!
families and communities.”
10 New Organizations Commit to the Healthcare Resiliency Framework
We are excited to announce 10 additional commitments to the Healthcare Resiliency Framework attained this quarter. The LAN, with the support of the Executive Forum members, has secured commitments from a range of healthcare organizations – including state governments, health plans, large and small health care providers, and large employers – to pursue many of the reforms outlined in the LAN Healthcare Resiliency Framework.
We would like to thank all 51 organizations that have signed the Shared Commitment Statement. This quarter, we are fortunate to add the following organizations to the growing list of organizations that have committed to the LAN Shared Commitment:

- Alliance for Technology Driven Health (ATDH)
- Archway Health
- Evolent Health
- Healthcare Information and Management Systems Societies (HIMSS)
- Leavitt Partners
- National Association of ACOs (NAACOS)
- National Partnership for Women & Families
- Network for Regional Healthcare Improvement (NRHI)
- Oregon Health Authority (OHA)
- Primary Care Collaborative (PCC)
Alliance for Technology Driven Health (ATDH)

The Alliance for Technology Driven Health (ATDH) represents health systems, medical groups, and technology companies with a goal of enhancing the visibility of the role technology and data in the value movement and critically evaluating the tools, partnerships, and processes necessary to implement capitated payment models. Our Allies are leaders in both Washington, D.C. and in national markets driving discussions with plans and providers to increase awareness and to provide the necessary tools to participate in performance-based payment models.
ATDH is committed to ensuring a resilient healthcare system that continues to prioritize high-value patient care. The unprecedented COVID-19 pandemic highlighted areas for improvement within the US healthcare system, as well as areas that can be further leveraged. ATDH believes a continued focus on transitioning to value-based payment models will not only strengthen the healthcare system but provide a robust foundation for any future event that puts pressure on providers and patients.
Our coalition will continue to serve as a resource for providers and other stakeholders interested in accelerating the transition to value-based payment models and the role technology plays to support providers interested in and already engaged in capitation arrangements.
Learn more at: https://techdriveshealth.org/
Archway Health

Archway Health has been collaborating with provider partners to achieve success in value-based care (VBC) programs since 2014. Through advanced analytics, clinical process improvement and shared financial risk, Archway has helped reduce healthcare costs and improve the quality of care for patients across the country, leveraging two-sided alternative payment models as a vehicle for change. The COVID-19 pandemic demonstrated that providers who had implemented VBC infrastructure and innovative care management strategies were better positioned to deliver high quality care amidst a public health emergency and underscored the importance of a better alternative to FFS reimbursement.
Archway continues its longstanding commitment to payment reform and proudly joins HCP-LAN in committing to the need for a resilient health care system. Specific actions Archway will carry out in this commitment include: 1) Expanding participation in HCP-LAN Category 4 population based alternative payment models (APMs), 2) Using our status as a certified CMS Qualified Entity to evaluate provider performance and identify and implement evidence based interventions to reduce health disparities and 3) Leveraging the experience and subject matter expertise of our provider partner community to advocate for improvements to APMs to better foster health equity.
Learn more about Archway here: https://www.archwayhealth.com/
Heath Care Transformation Task Force (HCTTF)

The Health Care Transformation Task Force (HCTTF) welcomes the opportunity to join the Health Care Payment Learning and Action Network in its commitment to transforming our health care system to one that provides value-based care that lowers cost, improves outcomes, and promotes equitable population health for individuals and communities. Now more than ever, our country’s health care system must be resilient in the face of challenges like COVID-19 while staying the course to move away from fee-for-service medicine.
As a consortium of payers, providers, purchasers and patient organizations, HCTTF was founded to advance its members commitment to pursuing value-based payment and care delivery models in both the public and private sectors, and to accelerate transformation across the health care system. Value-based care has the potential to address disparities and inequities that have long plagued our health care system and harmed disadvantaged populations, an unfortunate occurrence which has been on stark display during the current public health emergency. Value-based care can also heighten competition in ways that benefit all consumers and patients and forge strong partnerships among care delivery stakeholders.
HCTTF strongly believes value-based payment models should put patients at the center and coordinate their care in the most effective and efficient ways possible to address their medical, behavioral and social needs. The lessons that we have learned during the COVID-19 pandemic teach the importance of and need for a resilient and resourceful system to meet the unexpected challenges of the 21st century.
Learn more at: https://hcttf.org/
Leavitt Partners

Leavitt Partners’ mission is to improve lives by advancing value-based care, striving to make health more accessible, effective, and sustainable. Our organization supports the new LAN Healthcare Resiliency Framework which promotes multi-stakeholder collaboration to promote more resilient, effective alternative payment models.
Learn more at: https://leavittpartners.com/
Network for Regional Healthcare Improvement (NRHI)

The Network for Regional Healthcare Improvement (NRHI) is a national membership organization representing more than 30 regional health improvement collaboratives (RHICs) and affiliate organizations across the United States. RHICs share common strategies to address local priorities, including the transition to value-based payment models that can be used to improve our nation’s health system.
Our members are multi-stakeholder organizations that bring together healthcare providers, payers, purchasers, and consumers to collectively work towards achieving change. The NRHI network reaches approximately 70% of the United States.
NRHI members demonstrate practical, hands-on expertise and support the transition to value-based payment by:
- Bringing historical knowledge, market intelligence, and expertise in stakeholder engagement through providing opportunity to work closely with providers and clinicians in their regions
- Providing regional education and training and promotion of the HCP LAN Roadmap and resources and participating in HCP LAN activities
- Conducting direct technical assistance with practices and providers
- Delivering leadership and support for measurement and reporting
- Capturing lessons learned and barriers to implementation
- Identifying top levers across markets
- Offering influence from self-insured employers, as well as commercial and government entities
- Recommending refinement of tools, resources, and initiatives
- Designing and supporting payer alignment efforts
- Convening local payers and providers to support value-based payment efforts
- Compiling and submitting comments on draft payment rules
Learn more at: https://www.nrhi.org/partner-with-nrhi/
If you are interested in committing to the LAN Healthcare Resiliency Framework,
send us an email: hcp-lan@rippleeffect.com.
LAN Next Initiative: Primary Care Action Collaborative
As evidenced by the LAN Resiliency Collaborative, there is broad support among LAN Executive Forum members for advancing alternative payment model (APM) adoption, including shared/individual commitments to accelerate movement toward population-based APMs in primary care and an increased focus on health equity. There also is ongoing interest in translating this general support into momentum to accelerate adoption of more meaningful and effective primary care/population health models using LAN’s multi-payer and multi-stakeholder focus. The LAN will be launching a Primary Care/Population Health Action Collaborative (PC/PH AC) to accelerate adoption of resilient, population-based APMs with prospective cash flows for primary care providers and achieve more equitable outcomes in PC/PH APMs.
As a first step to achieving these objectives, the LAN anticipates launching a Health Equity Workgroup (HE WG). Stay tuned for more information as the LAN prepares to launch this work!

APM Measurement Effort Update
The LAN recognizes the national and global issues and uncertainty we face, as well as the impact the COVID-19 pandemic has on the healthcare industry and the partners of the HCP-LAN. To that end, the HCP-LAN is conducting the 2020 Measurement Effort in a way that gives maximum flexibility to health plans and participating states to respond to the survey on a timeline that makes sense for their business operations.
 The HCP-LAN will resume its regular annual Measurement Effort in the spring/summer of 2021 (collecting 2020 APM data). Both 2019 APM results and 2020 APM results will be released in the fall of 2021.
The HCP-LAN will resume its regular annual Measurement Effort in the spring/summer of 2021 (collecting 2020 APM data). Both 2019 APM results and 2020 APM results will be released in the fall of 2021.
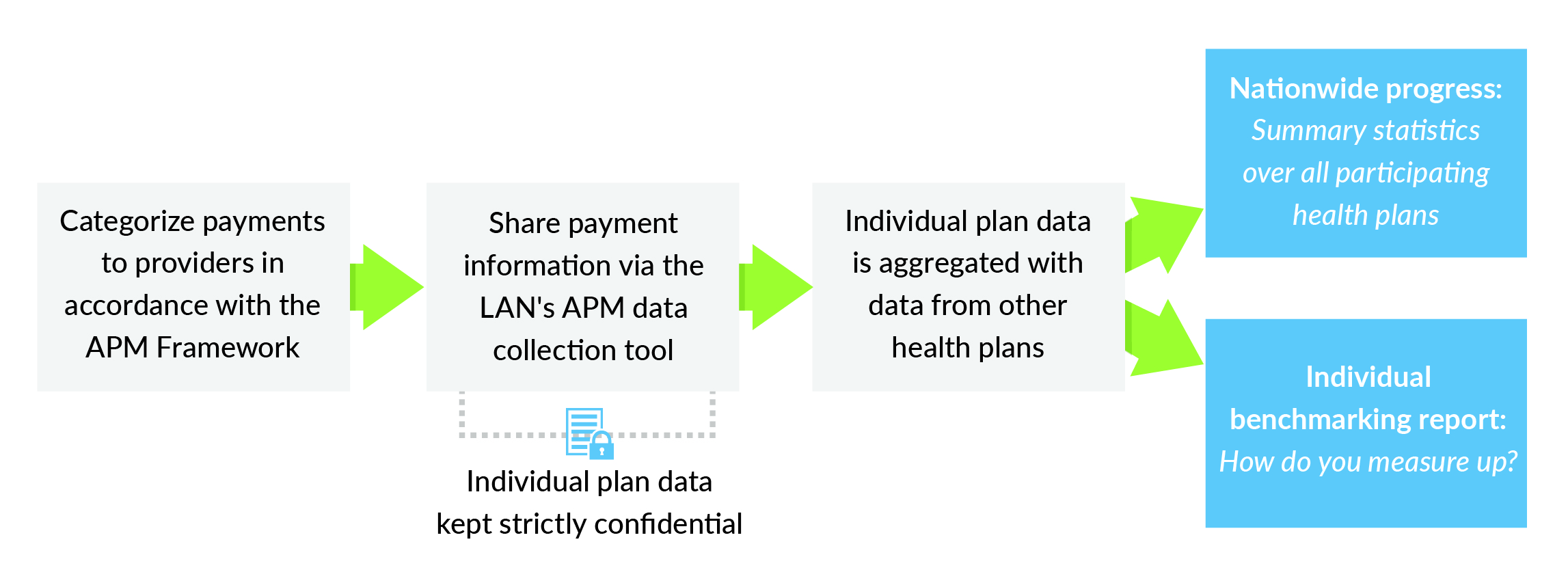
For 2021, participating payers will report total in- and out-of-network healthcare spending paid to providers through each of the categories and subcategories during 2020 or the most recent 12 months in the commercial, Medicaid and Medicare Advantage markets. The LAN works directly with participants to classify payments according to the Refreshed APM Framework. This makes participation as simple and straightforward as possible.
Individual payer data will be kept strictly confidential. It will not be shared with other participants or parties outside of the LAN data collection team. For reporting purposes, individual payer data will be aggregated with data from other payers.
For more information, click here: https://hcp-lan.org/apm-measurement-effort/
We invite health plans to participate in this effort to inform and bolster our understanding of nationwide progress toward APMs, as well as give you a better idea of where your organization stands in relation to other health plans.
If you would like to get involved in this year’s Measurement Effort, please contact us at hcp-lan@rippleeffect.com
LAN Leaders in the News
Co-Chair: Will Shrank, MD
READ: Health Costs and Financing: Challenges and Strategies for A New Administration“As 2021 begins, there is pressing need and opportunity to reform health care financing to better support access, affordability, and equity.”
Executive Forum member: Marshall Chin, MD, MPH, Farzad Mostashari, MD, Jaewon Ryu, MD
READ: The Future of Value-Based Payment: A Road Map to 2030“The 2020s require a new strategy that moves from a short-term focus on testing new payment models to a long-term focus on expanding models that are most likely to generate substantial savings and improve quality.”
Executive Forum member: ChenMed, Chris Chen, MD
LISTEN: What Mission-Driven Valued-Based Care Looks LikeIn the new ChenMed podcast, Faisel and Friends, Dr. Faisel Syed and his guests discuss the status of healthcare in America.
Co-Chair: Will Shrank, MD
LISTEN: Take Five with William ShrankWilliam Shrank, Chief Medical Officer, Humana, explains how strong payer-provider partnerships help advance patient care and drive successful value-based care models.
RESOURCES
- Healthcare Resiliency Collaborative home page:
https://hcp-lan.org/resiliency-collaborative/ - Shared Commitments:
https://hcp-lan.org/resiliency-collaborative/shared-commitment/ - Individual Commitments:
https://hcp-lan.org/resiliency-collaborative/individual-commitments/ - Executive Forums:
https://hcp-lan.org/executive-forum/
Our Vision
An American healthcare system that pays for value to the benefit of our patients and communities.
Our Mission
To accelerate the shift to value-based care in order to achieve better outcomes at lower cost.
Our Goal Statement
Accelerate the percentage of US healthcare payments tied to quality and value in each market segment through the adoption of two-sided risk alternative payment models.






















 Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models.
Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models. Mr. James Sinkoff is the Deputy Executive Officer and Chief Financial Officer for Sun River Health (formerly known as Hudson River HealthCare), and the Chief Executive Officer of Solutions 4 Community Health (S4CH); an MSO serving FQHCs and private physician practices.
Mr. James Sinkoff is the Deputy Executive Officer and Chief Financial Officer for Sun River Health (formerly known as Hudson River HealthCare), and the Chief Executive Officer of Solutions 4 Community Health (S4CH); an MSO serving FQHCs and private physician practices. Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System.
Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System. Dr. Brandon G. Wilson, DrPH, MHA (he, him, his) joined Community Catalyst as the Director of the Center for Consumer Engagement in Health Innovation, where he leads the Center in bringing the community’s experience to the forefront of health systems transformation and health reform efforts, in order to deliver better care, better value and better health for every community, particularly vulnerable and historically underserved populations. The Center works directly with community advocates around the country to increase the skills and power they have to establish an effective voice at all levels of the health care system. The Center collaborates with innovative health plans, hospitals and providers to incorporate communities and their lived experience into the design of systems of care. The Center also works with state and federal policymakers to spur change that makes the health system more responsive to communities. And it provides consulting services to health plans, provider groups and other health care organizations to help them create meaningful structures for engagement with their communities.
Dr. Brandon G. Wilson, DrPH, MHA (he, him, his) joined Community Catalyst as the Director of the Center for Consumer Engagement in Health Innovation, where he leads the Center in bringing the community’s experience to the forefront of health systems transformation and health reform efforts, in order to deliver better care, better value and better health for every community, particularly vulnerable and historically underserved populations. The Center works directly with community advocates around the country to increase the skills and power they have to establish an effective voice at all levels of the health care system. The Center collaborates with innovative health plans, hospitals and providers to incorporate communities and their lived experience into the design of systems of care. The Center also works with state and federal policymakers to spur change that makes the health system more responsive to communities. And it provides consulting services to health plans, provider groups and other health care organizations to help them create meaningful structures for engagement with their communities. Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.
Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.


 Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.
Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.








