Check out the latest resources from the LAN
New Resources
Working toward shared strategic goals, the Accountable Care Action Collaborative (ACAC), the Health Equity Advisory Team (HEAT), and the State Transformation Collaboratives (STCs) developed a suite of new resources that promote action, measure progress, and advance accountable care.
.Multi-Payer Alignment Blueprint
 The Multi-Payer Alignment Blueprint compiles successful multi-payer alignment initiatives from payers, providers, health systems, purchasers, patient advocates, and community organizations in the STC states—Arkansas, California, Colorado, and North Carolina.
The Multi-Payer Alignment Blueprint compiles successful multi-payer alignment initiatives from payers, providers, health systems, purchasers, patient advocates, and community organizations in the STC states—Arkansas, California, Colorado, and North Carolina.
The initiatives vary in scale and complexity and provide examples that other states can adapt and incorporate into their own multi-payer alignment efforts. The shared goals and approaches across these initiatives also provide a basis for generating cross-state alignment and building a foundation for national alignment.
Accountable Care Curve & User Guide
 During the 2023 LAN Spring Series, we unveiled our interactive Accountable Care Curve, a learning tool for organizations across the healthcare landscape looking to invest and advance in their journey towards accountable care.
During the 2023 LAN Spring Series, we unveiled our interactive Accountable Care Curve, a learning tool for organizations across the healthcare landscape looking to invest and advance in their journey towards accountable care.
The Curve includes the resources, articles, and papers that ACAC members used to guide their own transformation efforts and can help inform a tailored approach to enhancing capabilities for driving accountable care.
For a detailed overview of the levels of transformation, measurement tracks, milestones, organizational capabilities, and resources, as well as how to use this learning tool, see the Accountable Care Curve User Guide.
Learn MorePartnering with Community-Based Organizations
 New from the HEAT — “Guidance for Health Care Entities Partnering with Community-Based Organizations: Addressing Health-Related Social Needs in Alternative Payment Models”.
New from the HEAT — “Guidance for Health Care Entities Partnering with Community-Based Organizations: Addressing Health-Related Social Needs in Alternative Payment Models”.
Based on interviews with community-based organizations (CBOs) and other partners, this document provides guidance for health care entities on partnering with CBOs to address health-related social needs (HRSNs). The document features real-world examples and recommendations for forming partnerships with CBOs that provide HRSN benefits and services to patients, families, and their communities.
2023 APM Measurement Results
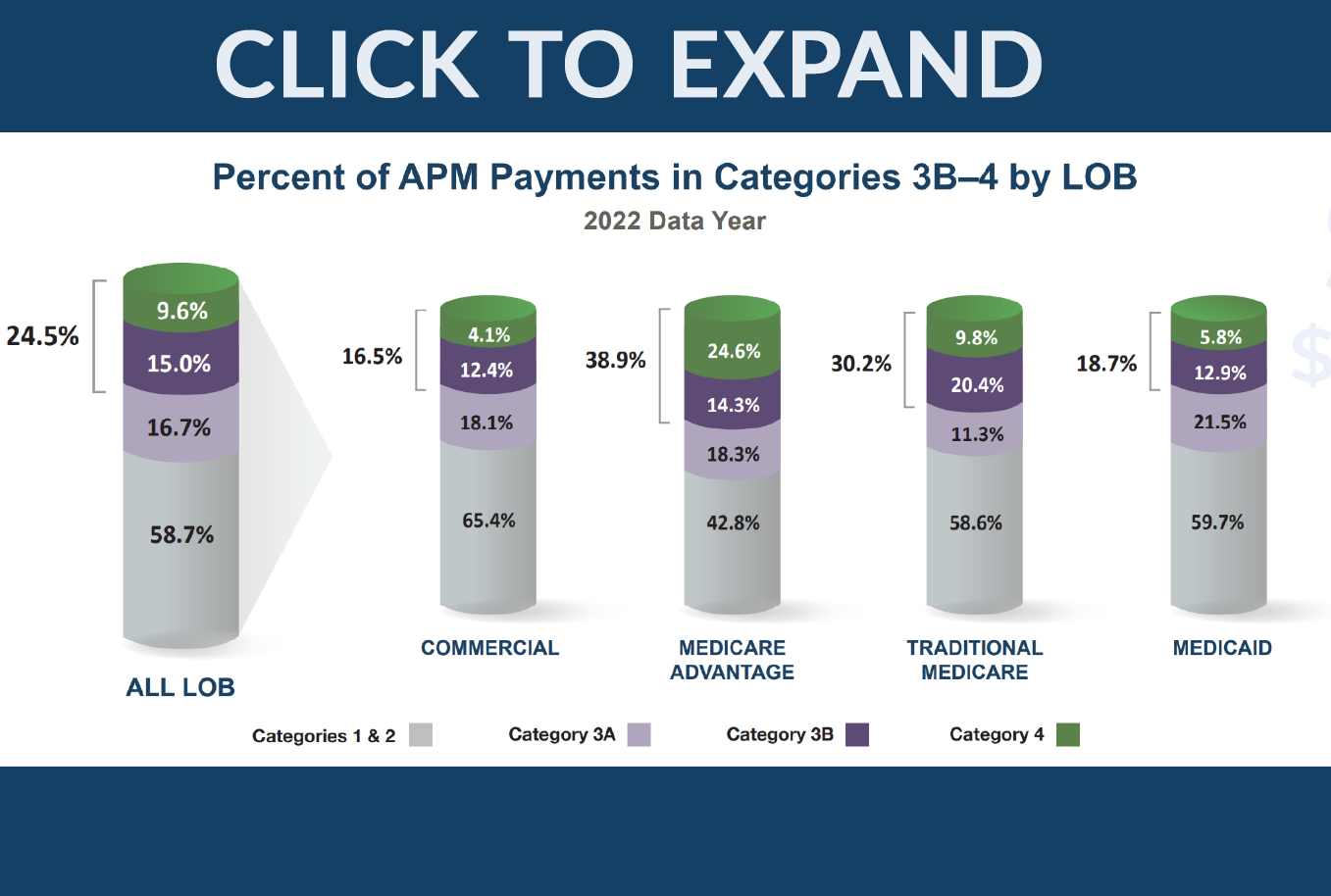 The 2023 APM Measurement Results indicate steady progress in the adoption of alternative payment models (APMs) across all lines of business (LOBs) ― Commercial, Medicare Advantage, Medicaid, and Traditional Medicare―with payers increasing their investments in value-based models. Two-sided financial risk arrangements (categories 3B and 4 in our framework) grew over 5 percent this year and accounted for 24.5 percent of all U.S. health care spending.
The 2023 APM Measurement Results indicate steady progress in the adoption of alternative payment models (APMs) across all lines of business (LOBs) ― Commercial, Medicare Advantage, Medicaid, and Traditional Medicare―with payers increasing their investments in value-based models. Two-sided financial risk arrangements (categories 3B and 4 in our framework) grew over 5 percent this year and accounted for 24.5 percent of all U.S. health care spending.
We also introduced metrics across all LOBs aimed at counting the lives in a care relationship with accountability for quality and total cost of care.
For the full 2023 APM Measurement Survey results, review the 2023 Methodology and Results Report.
New to the APM Measurement Effort? Click here to learn more about our APM Framework, the industry standard for how payers and providers design APMs and set value-based goals.
Featured 2023 LAN Summit Highlights
Miss any of the 2023 LAN Summit? Session recordings are available on our website!
CMS’s Approach to Multi-Payer Engagement and Delivery System Reform
 CMS directors joined together to discuss how their respective centers are promoting value-based care and engaging payers across the system to achieve health system transformation and improve the care experience for patients.
CMS directors joined together to discuss how their respective centers are promoting value-based care and engaging payers across the system to achieve health system transformation and improve the care experience for patients.
- Dr. Meena Seshamani shared how the Center for Medicare (CM) is focusing on how to care for the person rather than just treat a disease. On the Medicare Advantage side, for example, CM streamlined prior authorization so that the plan follows local and national coverage that stays with a patient for the duration of their treatment, even if they change plans.
- Dr. Dora Hughes discussed Center for Clinical Standards and Quality’s (CCSQ) mission to promote high-quality, safe, and equitable health care for all CMS beneficiaries. She described CCSQ’s plans to expand the number of patient-reported outcome measures in the Merit-based Incentive Payment System, or MIPS, program.
- Daniel Tsai emphasized that maintaining health care coverage is a “huge priority” for CMS, particularly as states navigate post-pandemic changes in their Medicaid programs.
- Liz Fowler introduced the Advancing All-Payer Health Equity Approaches and Development (AHEAD) Model, designed to strengthen collaboration between Medicaid and Medicare at the state level. This initiative aims to curb rising health care cost growth, improve population health and health outcomes, and address disparities through statewide accountability.
Enabling Action with the Individual at Top of Mind: Effective Integration of Patient and Caregiver Perspectives
 Panelists discussed the importance of considering the needs and perspectives of beneficiaries, patients, and family care givers when making decisions based on data, as well as the challenges caused by a lack of coordinated care.
Panelists discussed the importance of considering the needs and perspectives of beneficiaries, patients, and family care givers when making decisions based on data, as well as the challenges caused by a lack of coordinated care.
We also announced the Person Perspectives Council, a new initiative to amplify the voices of individuals, patients, and caregivers and reinforce our commitment to promoting whole-person, accountable care.
Enabling Aligned Action: Multi-Payer Alignment Strategies and Impact
 Dr. Alice Chen led an engaging discussion on promoting directional alignment and “balancing the desire for synergy with flexibility” among payers who are both collaborators and competitors. Payers should align on key aspects of value-based care that, when standardized, can significantly optimize care for patients.
Dr. Alice Chen led an engaging discussion on promoting directional alignment and “balancing the desire for synergy with flexibility” among payers who are both collaborators and competitors. Payers should align on key aspects of value-based care that, when standardized, can significantly optimize care for patients.
During this session, we announced the National Health Plan Workgroup, which will accelerate payment reform at the national and local levels by convening large national health plans and CMS to foster directional alignment across key components of accountable care.
Watch the Session
CBO Partnership
Read more: How Can APM Participants Better Engage Community-Based Organizations? | Healthcare Innovation (hcinnovationgroup.com)• This article highlights the 2023 LAN Summit HEAT panel on how health care executives can better partner with community-based organizations (CBOs) to address patients’ health-related social needs and decide on meaningful measures.
LAN Resources
Read more: Health Care Payment LAN to Increase Focus on Multi-Payer Alignment | Healthcare Innovation (hcinnovationgroup.com)• Referencing data from the 2023 LAN Summit, this article highlights the consistent growth in alternative payment methods across the U.S. health care industry, the Multi-Payer Alignment Blueprint, the Accountable Care Curve tool, the National Health Plan Workgroup, and overall goals for the upcoming year to reinforce health equity efforts.
APM Measurement
Read more: New Survey Demonstrates Health Care’s Continued Commitment to Value-Based Care Models – AHIP• America’s Health Insurance Plans (AHIP) issued a statement regarding the APM Measurement survey results, designed to illustrate how widely value-based care models are being adopted as health insurance providers, clinicians, hospitals, and health care systems work together to transition from paying for volume to value.
Read more: Value-Based Reimbursement Grows as Providers Take on More Risk (revcycleintelligence.com)
• This article outlines the APM Measurement Effort results, stating that “this year’s ‘APM Measurement Effort’ found that just 40.6 percent of payments across public and private payers were strictly fee-for-service. Meanwhile, 18.1 percent of payments had some link to quality and value.”
Read more: Value-Based Care Bending Cost Curve and Gaining Momentum (leadingage.org)
• This article summarizes the 2023 LAN Summit and CMS renewed commitment to shifting all Medicare beneficiaries to accountable care models by 2030 and acceptance that managed care will be a growing proportion of the future of payment.
Read more: Value-based care growth stagnant in 2022 (beckerspayer.com)
• Our annual report, as referenced in this article, highlights that the adoption rate of value-based care models remained consistent from 2021 to 2022. However, there was a notable shift in funding, with more dollars moving to two-sided risk-based models.
Our Vision
An American healthcare system that pays for value to the benefit of our patients and communities.
Our Mission
To accelerate the shift to value-based care in order to achieve better outcomes at lower cost.
Our Goal Statement
Accelerate the percentage of US healthcare payments tied to quality and value in each market segment through the adoption of two-sided risk alternative payment models.


















 Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models.
Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models. Mr. James Sinkoff is the Deputy Executive Officer and Chief Financial Officer for Sun River Health (formerly known as Hudson River HealthCare), and the Chief Executive Officer of Solutions 4 Community Health (S4CH); an MSO serving FQHCs and private physician practices.
Mr. James Sinkoff is the Deputy Executive Officer and Chief Financial Officer for Sun River Health (formerly known as Hudson River HealthCare), and the Chief Executive Officer of Solutions 4 Community Health (S4CH); an MSO serving FQHCs and private physician practices. Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System.
Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System. Dr. Brandon G. Wilson, DrPH, MHA (he, him, his) joined Community Catalyst as the Director of the Center for Consumer Engagement in Health Innovation, where he leads the Center in bringing the community’s experience to the forefront of health systems transformation and health reform efforts, in order to deliver better care, better value and better health for every community, particularly vulnerable and historically underserved populations. The Center works directly with community advocates around the country to increase the skills and power they have to establish an effective voice at all levels of the health care system. The Center collaborates with innovative health plans, hospitals and providers to incorporate communities and their lived experience into the design of systems of care. The Center also works with state and federal policymakers to spur change that makes the health system more responsive to communities. And it provides consulting services to health plans, provider groups and other health care organizations to help them create meaningful structures for engagement with their communities.
Dr. Brandon G. Wilson, DrPH, MHA (he, him, his) joined Community Catalyst as the Director of the Center for Consumer Engagement in Health Innovation, where he leads the Center in bringing the community’s experience to the forefront of health systems transformation and health reform efforts, in order to deliver better care, better value and better health for every community, particularly vulnerable and historically underserved populations. The Center works directly with community advocates around the country to increase the skills and power they have to establish an effective voice at all levels of the health care system. The Center collaborates with innovative health plans, hospitals and providers to incorporate communities and their lived experience into the design of systems of care. The Center also works with state and federal policymakers to spur change that makes the health system more responsive to communities. And it provides consulting services to health plans, provider groups and other health care organizations to help them create meaningful structures for engagement with their communities. Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.
Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.


 Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.
Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.








