EPISODE 2: Meeting Patients Where They Are: A Community-Based Approach to Overcoming Health Barriers, Featuring Dr. Andrea Gelzer and Karen Dale, AmeriHealth Caritas
“The time is now. We have all the lessons we’ve learned from the pandemic in how swiftly we can move when we have a sense of urgency.” — Karen Dale, Market President, AmeriHealth Caritas District of Columbia
Host Jeff Goldman, Director of the LAN through the MITRE-operated Health FFRDC, interviews Dr. Andrea Gelzer, Senior Vice President and Chief Medical Officer for AmeriHealth Caritas and a member of the LAN’s Care Transformation Forum, and Karen Dale, Market President of AmeriHealth Caritas District of Columbia and Co-chair of the LAN’s Health Equity Advisory Team (HEAT). In this episode, they share how their organization is responding to issues of equity and access while promoting value-based payment initiatives to improve outcomes.
Episode Q & A
(01:41) For our conversation today, we're going to focus on three critical topics and how they intersect with each other. They are value-based care, equity, and alternative payment models (APMs). I'm going to direct the first question to Andrea. Can you tell us a bit about AmeriHealth Caritas’ current value-based care initiatives?
Dr. Andrea Gelzer:
AmeriHealth Caritas really is continuing to make positive strides to help transition providers from a fee-for-service model to one of our value-based alternative payment models. Across our markets, almost 90% of our members are receiving care from a provider that participates in one of our alternative payment, or as we pin them, “perform plus” programs. In 2020, we continued to see more providers actually advance to more advanced alternative payment models, in a category three or four payment model. And that’s a metric that has increased significantly year over year since 2017. We still continue to see the largest growth in the 3A models or the shared savings models. In 2020, nearly 15% of our value-based arrangements were in categories 3B and 4. So those are the advanced payment models where providers begin to take downside risk. And that’s a good improvement I would say. We anticipate that this is going to increase for our 2021 LAN APM measurement survey results next year as well. We’re seeing some health systems interested in category 4 APMs and also some interest from specialized provider types including substance use disorder providers and behavioral health providers who are ready, to accept downside risk. I think that’s exciting. Unfortunately, that’s not the case for all, and provider interest in downside risk for a Medicaid population continues to be a significant hurdle we have yet to overcome. Today we’re leveraging our perform plus programs to improve social determinants of health, health, equity, and access to healthcare in the communities we serve. We’ve incorporated incentives for reporting of Z codes for social determinants of health into our value-based programs, and really continue to see an increase in provider reporting.
(04:46) Karen, could you talk a little bit about your health equity strategy and how that connects into the value-based care strategies that Andrea just described.
Karen Dale:
So, let me begin with, how are we defining equity? Equity is ensuring that people have what they need to grow, thrive, and be resilient. So that means we must meet them where they are, not where we would wish to begin. And so that’s part of the transformation in terms of our healthcare delivery system. Where alternative payment methods come in, is giving that level of flexibility, support, and engagement with providers and other components of our healthcare delivery system to ensure people are getting what they need. So, for example, as we think about the maternal health crisis for women of color, if we have a way of incentivizing or doing a bundled payment or coming up with a mechanism that supports nurse practitioners, obstetricians, to be connected to community-based organizations, to have more time to do screening, and engage peer support for moms to be more healthy. We’re now creating this additional delivery system so that these women, who have more complexity socially, possibly more complexity medically, are getting all those wraparound services, supports, and connections that improve health outcomes. So that’s a more equitable approach that alternative payment methods can help us to create. And so, we can think about that in so many ways. What did we learn with the pandemic? We learned that we weren’t thinking about how to use the data to inform an equitable approach to what we were going to do, right? So, knowing that people of color were more likely to have diabetes, hypertension, high cholesterol, heart disease, all those things. If we were taking the equitable approach, we would be thinking, “so how do we address that within a payment framework to create different outcomes” rather than reacting after and saying, “oh my goodness, look at the disproportionate negative impact in communities for people of color.” So alternative payment methods have just great potential to be that catalyzing force around how we engage with providers differently, how we connect them with community-based organizations, how we meet people where they are by providing the additional information, healthcare delivery, and other supports to improve health outcomes and decrease costs.
(07:38): What are some of the biggest challenges that you face in implementing health equity initiatives? Can APMs help overcome those barriers or are there other ways that you're overcoming those barriers?
Karen Dale:
One of them, for certain, is even though providers may be engaged and interested, how do they build that into their workflows and their offices and their practices? FQHCs (federally qualified health centers), they get kind of the funding they need already in many ways to have team-based care. And you may see that as well with some of the mid-size providers. When we get to the much smaller providers that becomes more challenging. How do we create the best synergy between what a payer offers and can do to support practices and giving them more ability and funding through the alternative payment methods to do things differently and adjust their workflows? One of the places that payers can be extremely useful is the data and information that we can provide. We have to serve it up in a way that’s easily consumable and leads to the providers taking action at the point of care doing a visit. Today, it’s a little uneven. We’re still working through how to do that well; however, that does present a pain point: how to make this work in a way that works for the provider, works for their patient, our members that are presenting for care. Data is another piece. Andrea mentioned “Z” codes. Though we add an incentive in our methods for paying providers or reimbursing them for that, sometimes they say it’s too much. It’s one more thing to do. How do we make it as easy as possible for that to occur? Finally, providers really … some of them don’t have the bandwidth to look at the data, to use it, they say that makes things longer, they’d rather spend more time with the patient. So, we’ve got to figure out in the technology space, how do we make it easier? How do we make the data transfer more democratized so that we get what we need, they get what they need, in a way that moves us forward with what our patients need? And today we’re still all working through that. I’m a fan of HIEs (health information exchanges) that are well-funded in states that allow for that place and space where rather than people having to go into several different systems to get information about what is going on with their patient, our members, that there’s more of a place where anyone and everyone that is part of the healthcare delivery system can go. And then if I think about payers, that’s another component where the more we are aligned across payer type, so that the things that we are asking for or using, from a provider facing standpoint, it reduces that provider administrative burden and allows for them to probably be more interested in participating and making changes.
Dr. Andrea Gelzer:
I would just add to that Karen, that, we’ve been talking about care transformation and the LAN for quite some time and giving providers the right tools, giving them the right data, putting them in a position to truly succeed. Not only from a financial point of view, but also succeed in improving health outcomes through moving to these more advanced models. And I would say one thing that the pandemic has shown us is that providers are truly resilient, and they have embraced telehealth, they’ve embraced virtual care. So, I hope that they are embracing, and I know that they are embracing different ways to incorporate all of these important elements to assure and improve healthcare from an equity basis going forward.
(12:16) How does AmeriHealth Caritas collect and use socio-demographic or other data to support the design or the execution of your APMs or your health equity strategy overall? We hear a lot about the challenges of having good data to support these kinds of models and wondering what kind of work you all have done to advance that.
Dr. Andrea Gelzer:
We look at our data and any data that we’re able to obtain from multiple sources from a lot of different angles. We look at race, ethnicity, language, age, location, for example. We’ve been collecting race and ethnicity and language data from our members for at least 10 years. And we’ve been collecting social determinant data since — in a very structured fashion — since 2017. We’re beginning to collect data related to sexual orientation, gender identity. A lot of the health equity focus is around race, ethnicity, language, but other populations face barriers to care too, including the LGBT populations. We also track social determinant health needs across 14 different domains, and then we’ve got information now from about at least 25% of our households. We’re also working with The Gravity Project to help assure that the data we collect, and the data other payers collect, and the data providers collect, is collected in a similar manner so that we can close the loop on collecting the data, addressing the need, improving the health outcome. We understand that healthy behaviors and outcomes are impacted by socio-demographics, so we’re trying to thoughtfully align our policies and programs to best serve our members and communities. For example, we use the socio-demographic data that we collect to help identify potential disparities, and we overlay that data with race, ethnicity, language data to identify trends within specific populations. And we provide targeted outreach and programs to members to hopefully improve health outcomes in underserved communities. We try to promote more culturally linguistically diverse provider networks. And we try to build strong relationships with trusted community-based organizations to improve social, physical and economic environment.
(15:28) You mentioned earlier that providers are coming from a mix of different sort of perspectives and capabilities. Are there specific programs you've found effective at helping to bridge and helping to build partnership and capability with providers so that you can have a greater impact on equity and greater participation and success in APMs.
Dr. Andrea Gelzer:
We work a lot with federally qualified health centers, and I think that National Association of Community Health Centers and in the primary care associations in the different markets we serve have been really helpful in supporting their membership. We also have implemented programs where we actually embed health plan staff in a practice like one day a week, or however much they need us, to try to work with the staff ourselves. So, it’s really a combination of external sources and also the AmeriHealth Caritas resources to help bring providers along.
Karen Dale:
Where we’ve seen providers really make great strides is when we’ve had embedded staff because they’re right there helping to problem solve, to engage with members, to follow up, make the necessary connections and reinforcements. And so again, it frees up some of their provider resources. So that’s been really successful. The other component is, it’s all about making it easy, right? If a provider simply needs to let us know what they found in a visit — that someone is housing insecure, food insecure, whatever the challenges are. When we can easily pick up on that thread and address a need, providers find that incredibly useful because they’re not necessarily staffed other than some of the FQHCs to make those things immediately happen. So, it’s that partnership and collaboration of us picking up and doing what we do well, which is connect the dots and perform expert care coordination. That really helps to move us towards equity. It helps providers to lean in knowing that they have that stable support and engagement as well.
(18:34) Because you talked about connecting providers to community-based organizations and helping to bridge that gap from the healthcare system to the public health system I'm wondering if there are things that you do to interface with the community-based organizations to help foster that connection from, not only identifying a gap in, say, housing or food or transportation, but actually connecting folks to local services that can help fulfill those gaps?
Karen Dale:
There are several platforms out there, Now Pow, Unite Us, Aunt Bertha, that are enablers, that again, help us to do this work better. So, we’re not starting from scratch. Back to the concept of democratization, ensuring that members can access things themselves is incredibly empowering. It also helps to decrease stigma, because sometimes I don’t want to tell the person on the other end of the phone, who’s really a stranger, that I don’t have food. They may tell their doctor because they’re sitting right there in the office and their blood glucose levels are off or whatever, right? Enabling our members, doctors, patients to be able to take action on their own is really important in terms of our work around equity. Allowing the provider to be able to quickly make a referral or connect someone to a resource is equally important, so just in that moment, something different can happen that will help to influence a positive outcome or avoid something like an emergency room visit. Using enablers, such as those types of platforms, as an important component, in terms of that connection to community-based organizations. It’s equally important that the community-based organizations know how the healthcare delivery system on a payer’s side works, which we should have done that some time ago. Now that we all understand social determinants of health and all of that, working to educate them about how important their role is and how important it is that they help us close the loop. So did that person show up and what service did they get? And so then we have even more rich data that tell us: what are those top three things that people are needing? We can now be more specific in our efforts to work on policy and advocacy that also helps to advance and create the change. In the District (Washington, DC), for example, the east end of our city has much poorer health outcomes. When we’ve looked at block-by-block data, we know that there are places where there’s a lot more food insecurity and there are a lot more people with diabetes, hypertension, high cholesterol. So what does that tell us? Well, if we are partnering with community-based organizations that are located right there, that makes it easier for people to access what is needed and for us to create the change. If we invest in helping them by us being there, like we’ll have some of our community health workers there, that kind of thing, then all of a sudden now we’ve got this community of change and support that’s moving people to better health outcomes. And so, it’s work that we love doing; it ties with our mission. The data that comes from what we get from multiple sources, as well as using alternative payment methods really helps us to move things forward.
(22:14) Are there initiatives coming out of the state Medicaid agencies in your markets that are supporting or helping to drive or creating opportunities to focus even greater on health equity or [to] share information?
Dr. Andrea Gelzer:
I would say there are health equity initiatives now coming from every state Medicaid agency. But they’re coming as expectations for the plans. So they’re coming not as a request, but it’s like everyone is trying to address health equity, trying to address social determinants, trying to address disparities. And there is certainly a renewed interest. No one has the silver bullet. I think that we’re all working together and, as I started my answer, it’s really expectations that we’re seeing. And I think that every state is looking for solutions to this. So that’s why it’s so important that multi-stakeholders sit in the same room and try to work on these issues to impact outcomes.
Karen Dale:
I agree with Andrea on the kinds of expectations we’re seeing, such as, there has to be a dedicated key position that’s responsible for health equity at a plan level. There’s someone accountable that the state can know must have a plan. We’re seeing requests to have a specific plan with measurable information. There’s some common issues that emerge, such as maternal health outcomes for women of color, that there’s an expectation that the health plans can focus their efforts, align with community-based organizations and policies that help to advance that, such as, whether doulas are being reimbursed. Do you have meal delivery programs, peer supports for moms? How are you building this flexible system that meet women where they are and reduce their risk? In the District, for the first time this fiscal year, our budget was reviewed with a health equity lens. So it said, whom would we leave behind if we didn’t do X? And how do we create not just policies, but how do we create the right momentum by aligning things to ensure that we’re addressing those with the most need? And so it covered everything from what else we need to do around maternal health outcomes to what are we going to do to support the emotional wellbeing for those children who were already experiencing multiple emotional and educational challenges during the pandemic? So that as they go forward, we have a process in place for more in-school support to help close the gap on what may have been eroded during the pandemic. And so, I applaud those efforts, their early days, as we’re all learning how to work together in different ways towards the same common goals and purpose. I’m excited by the fact that we are talking about it. Organizations are leaning in to say, here’s what I can do, here’s what I think, saying that we can do this together. It takes lots of components, certainly, but the pandemic also taught us how quickly we can mobilize to change policies and get things done and hopefully that’s a carry forward.
Dr. Andrea Gelzer:
And I’m excited too that the states seem to be taking a much more realistic approach to this. They’re not telling us we must address social equity in any one way. I think there’s a lot of hope here that this approach, allowing us to innovate, explore, and truly be impactful and may make a difference. We’ve been at this for a long time.
(27:27) I want to shift gears for a moment and talk a little bit about alternate payment models, which we talked a little bit about at the top of our conversation. What type of models are best suited for promoting health equity, and how can models be designed to be deliberately focused on getting measurable change in health equity?
Dr. Andrea Gelzer:
I think that whatever the model to promote health equity, they’re always quality gates in a model. And I believe that whatever the alternative payment model, if it’s a population-based model with quality gates, those quality gates have to include measures of health equity. I think we’re still nascent in which of those measures truly drive outcomes, but including them is a very good first step. Because outcomes alone, aren’t the only measure. You have to take a really deep dive into the outcomes and you also have to make sure that you look at the outcomes and stratify them by race, ethnicity, language, social determinants. So if providers may meet benchmarks for one certain population, but their performance is lagging compared to the population at large, there’s still an equity issue. So we’re using this approach by taking existing quality measures and really bifurcating the baseline data by race, ethnicity, and language to look at opportunities for improvement. I’ll give you an example. Docs earn more if they improve access to care metrics for the African-American population if a disparity exists for that population. So really target the incentives to produce improved outcomes for the population where the performance measure is lagging.
Karen Dale:
When we think about the models, having quantitative and qualitative data. We need to ensure that even though we, the payer, and the provider may believe that they’re doing the best job, that we also hear from those we serve. And so how do we get their voice into the conversation, into the process so that we know whether they are seeing the benefit that we hope we are achieving.
Dr. Andrea Gelzer:
And how do we assure that from whoever, whichever members’ perspective that they feel as though their question got answered. They were respected. They had a good outcome.
(30:54) Are there particular challenges that you have faced in trying to roll out the models that are particularly focused on health equity in the markets where you operate?
Dr. Andrea Gelzer:
I think we’ve talked about the barriers before, that providers aren’t ready, or as Karen noted, you’re adding on something for them to do that they don’t particularly have time to do because of their workflow issues. I think it’s still too early in the game. I think really, we all need to get better at designing alternative payment models to really deliver the results and to work and respect the providers as well as our members to see that those programs are successful.
Karen Dale:
There’s like a push-pull between what we need or believe we need in terms of administrative things, so how do we reduce any of that to make it more likely that providers can see themselves engaging fully around alternative payment models, especially those that focus on equity? For example, if the concept of “gold carding” was used more often where prior auths (prior authorizations) have been approved 98, 99 percent of the time. Do we continue to ask that provider to do prior auths for whatever the specific area is? Or do we say, based on your history, you’re gold carded, and we’ll do retrospective audits? And that may help the provider to see themselves one, as a partner with the payer, and two, saying, “oh, so the time that was spent on that, I can now free up a resource or get a resource in my office that would focus more on these other things” that are advancing equity.
(33:21) How important do you all believe that multi-payer alignment is to advancing and accelerating adoption of alternative payment models?
Dr. Andrea Gelzer:
We have heard from providers for many years and continue to hear from providers about administrative burden and how each of the alternative payment models in which they participate has a slightly different quality metric. So they’re all measuring about the same thing, but it’s not exactly the same thing. And they have to collect information in one certain way for one payer, in one certain way for another. You talk about a push and pull Karen, it’s really a push and pull with providers and payers, and especially in Medicaid where providers want to be measured on the same thing. If you’re a multi-state Medicaid managed care entity, every state is measuring certain state-specific metrics. The quality metrics in every population, the quality metrics in every state, the ones that are most important to improve, they’re always going to be some differences, they’re not always going to be the same. It’s almost like the Holy Grail is the multi-payer collaboration because plans compete on the proprietary nature of their alternative payment models and how they deliver improved health outcomes. I think that we’re seeing state Medicaid agencies encourage multi-payer alignment on measures whenever possible. We participated in CPC+ in Louisiana and there was multi-payer alignment that was successful for things like developing a small core parsimonious measure set alignment on the way we reported data, common definition of data elements, and the creation of a learning collaborative for the participating payers. But I will tell you the take-up on that program unfortunately was not high enough to really move the needle. But those are the things that I think that we should be collaborating on, and it leaves us room to still have our own proprietary programs.
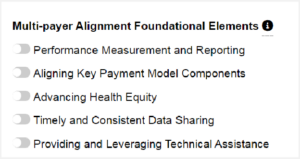
(36:45) Are there areas where national guidance or alignment would really be helpful to you and your markets as you try to move the needle along and try to spur along some of this multi-payer alignment or greater alignment in the markets?
Karen Dale:
Yes. If to the extent that the data sets were the minimum data sets that are required were clearly articulated. It just makes it easier because then the states would probably align more because of that clarity. And then that would be the expectation set with the payers. Right now, with everyone reinventing the wheel and coming up with so many variations, it’s impeding the rate at which we can get more adoption and then progress. I think starting with the data sets would be a great way to get greater alignment. What are we looking at for social determinants of health? What are we looking at in health risk assessments? Just all of that. If it were minimum, these are the things that everyone must collect, it would help move us forward. And we’d have so much of a better ability to measure and analyze and say what’s working, what’s not and why, if those data sets were consistent.
Dr. Andrea Gelzer:
Oh, I think that’s absolutely right, Karen. And we’ve been a supporter of Gravity since its inception, looking at how we collect social determinant data. I think that’s a great example too of a multi-stakeholder collaborative, where everyone’s sitting at the table trying to reach consensus on how we collect these data.
(38:57) Can you talk a little bit about some of the unique things that you guys are doing, and some of the things, from your perspective, that you've seen that you think would be great lessons learned?
Karen Dale:
As we think about equity, and it’s certainly top of mind for me coming out of the pandemic. Sixty days after the pandemic ends, it’s very likely we’ll have this tsunami, in terms of evictions, across the country. We know that housing is a stabilizing force for communities and people that we serve. And we know that in many of the communities that are going to be most affected, they won’t have representation. So, what happens next? This is the kind of thing that gives us an opportunity to utilize an equity lens. And what can we do? So, what if you have an entity, like in the District we have the Children’s Law Center, we have DC legal aid. What if we were reimbursing them and looking at outcomes in terms of how they might prevent evictions? We can come up with ways to address things that are challenges, health-harming when not addressed by using alternative payment methods for even other types of organizations that I call “health-adjacent” because they’re still important to what we’re trying to accomplish around health and health outcomes. Similarly, you think about, where we may need respite housing, right? For someone who is able to be discharged from the hospital can go home with health support; however, they’re experiencing homelessness. If we don’t address that, then they are readmitted, we’ve got more cost in the system than needed. What if we have a place where they can go, and that place has a value-based or alternative payment models. So we have one of those, which is awesome. And we’re looking at one with, one of our organizations that supports moms in terms of providing peer support, which is almost always in-person in some way, or over Zoom these days. So that when they produce better health outcomes — more babies that are full term, more moms that kept all of their appointments, all of those kinds of things—become the measures of whether they’re meeting the quantitative and qualitative measures in an alternative payment model. Those are some things that are really exciting that we are starting to do that through a health equity lens show the promise of what we can achieve by thinking about things differently.
Dr. Andrea Gelzer:
We’ve also had a very positive experience participating in the Advancing Health Equity, Leading Care Payment, and Systems Transformation. It’s a national program supported by RWJ (Robert Wood Johnson Foundation). It’s a learning collaborative and through it we’re working with the state Medicaid agency in Delaware, along with a provider partner to design a value-based model that supports delivery system transformation to eliminate disparities in healthcare. Through this program, I think we’re not only learning about ways to close the equity gap to meet the needs in Delaware, but we’re also able to benefit from the best practices from other participating stakeholder teams nationwide.
(42:50) We're getting close to the end of our time. I'm going to offer both of you the opportunity for some closing thoughts.
Karen Dale:
The time is now. We have all the lessons we’ve learned from the pandemic in terms of how swiftly we can move when we have a sense of urgency. So, leveraging that knowledge, leveraging what we learned about the communities that were most harshly affected, we can certainly do better. Many things that we’re doing are at a starting point, even though we’ve been doing them for a long time. They’re not at full scale. And so, my hope for us all is that we keep leaning in and doing the hard work to create better outcomes. The people we serve deserve it, and we’re more than capable to put the energy, the time, the investment to make it happen.
Dr. Andrea Gelzer:
This is a long, but such an important journey. I think we’re making progress and I’m just going to give credit to the LAN. I think the LAN is a big reason for that progress because the LAN is helping us all to move along.


















 Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models.
Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models. Mr. James Sinkoff is the Deputy Executive Officer and Chief Financial Officer for Sun River Health (formerly known as Hudson River HealthCare), and the Chief Executive Officer of Solutions 4 Community Health (S4CH); an MSO serving FQHCs and private physician practices.
Mr. James Sinkoff is the Deputy Executive Officer and Chief Financial Officer for Sun River Health (formerly known as Hudson River HealthCare), and the Chief Executive Officer of Solutions 4 Community Health (S4CH); an MSO serving FQHCs and private physician practices. Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System.
Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System. Dr. Brandon G. Wilson, DrPH, MHA (he, him, his) joined Community Catalyst as the Director of the Center for Consumer Engagement in Health Innovation, where he leads the Center in bringing the community’s experience to the forefront of health systems transformation and health reform efforts, in order to deliver better care, better value and better health for every community, particularly vulnerable and historically underserved populations. The Center works directly with community advocates around the country to increase the skills and power they have to establish an effective voice at all levels of the health care system. The Center collaborates with innovative health plans, hospitals and providers to incorporate communities and their lived experience into the design of systems of care. The Center also works with state and federal policymakers to spur change that makes the health system more responsive to communities. And it provides consulting services to health plans, provider groups and other health care organizations to help them create meaningful structures for engagement with their communities.
Dr. Brandon G. Wilson, DrPH, MHA (he, him, his) joined Community Catalyst as the Director of the Center for Consumer Engagement in Health Innovation, where he leads the Center in bringing the community’s experience to the forefront of health systems transformation and health reform efforts, in order to deliver better care, better value and better health for every community, particularly vulnerable and historically underserved populations. The Center works directly with community advocates around the country to increase the skills and power they have to establish an effective voice at all levels of the health care system. The Center collaborates with innovative health plans, hospitals and providers to incorporate communities and their lived experience into the design of systems of care. The Center also works with state and federal policymakers to spur change that makes the health system more responsive to communities. And it provides consulting services to health plans, provider groups and other health care organizations to help them create meaningful structures for engagement with their communities. Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.
Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.


 Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.
Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.








