Accountable Care Definition
“Accountable Care” centers on the patient and aligns their care team to support shared decision-making and help realize the best achievable health outcomes for all through comprehensive, high-quality, affordable, longitudinal care.
Encouraging Action During Accountable Care
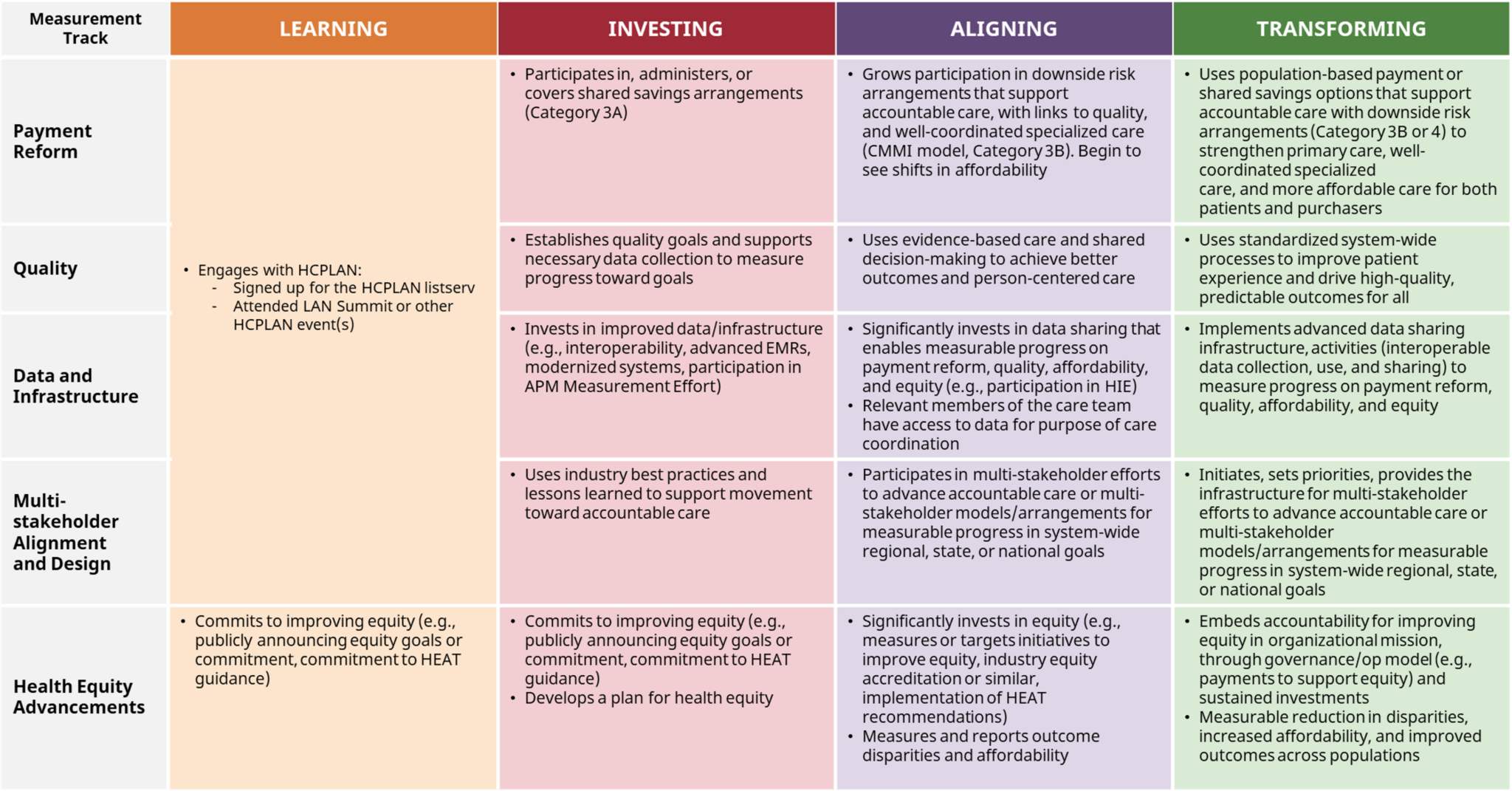
The Accountable Care Curve informs a tailored approach to enhancing stakeholder capabilities for driving accountable care.
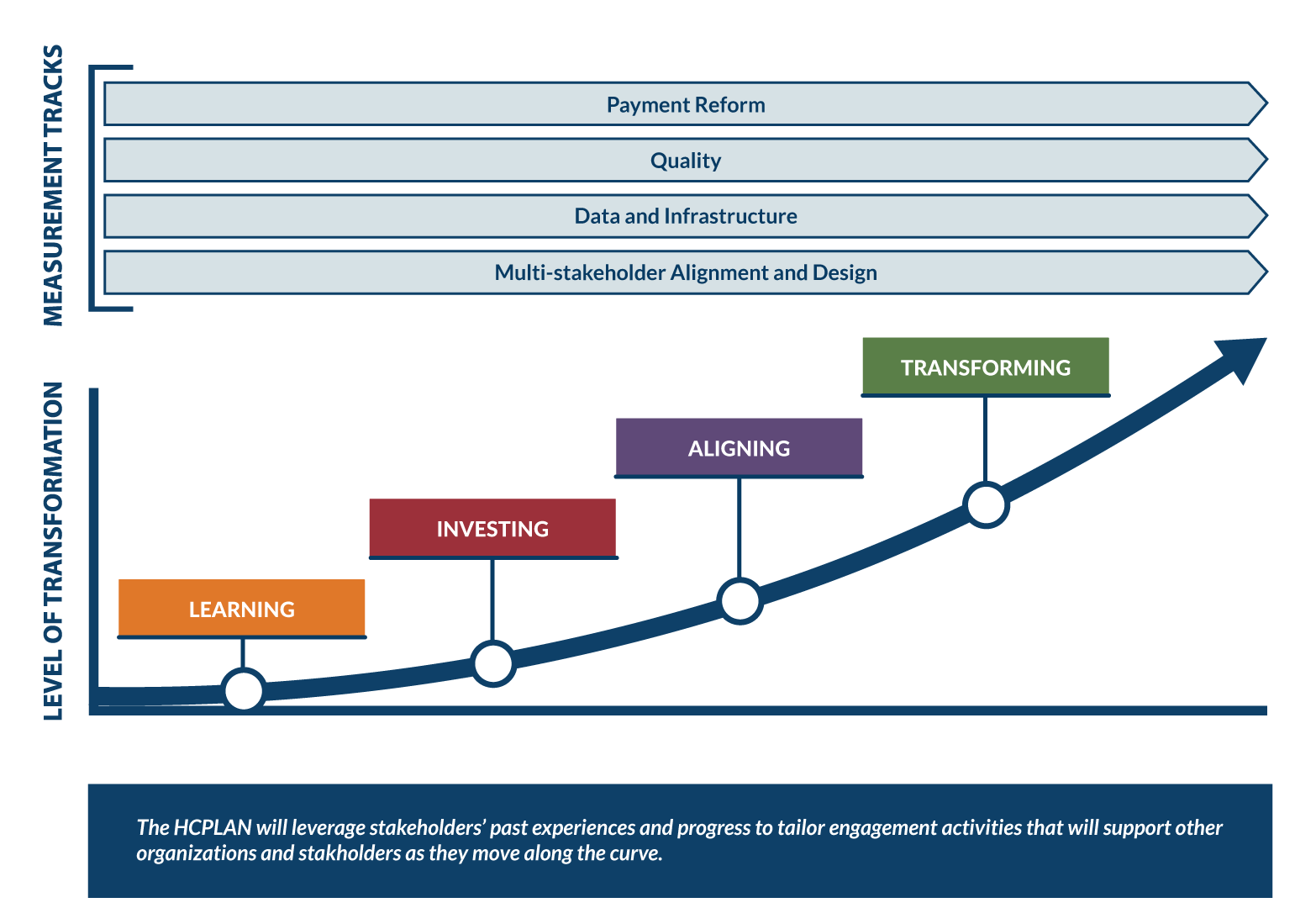
LEARNING
Organizations recognize the need for accountable care, understand the role they could play, and plan to act.
INVESTING
Organizations invest resources into achieving accountable care and demonstrate public support for industry promising practices.
ALIGNING
Organizations take action to align with industry best practices in accountable care, and consistently invest resources into achieving advanced accountable care.
TRANSFORMING
Organizations successfully shift their drivers and incentives toward advanced accountable care, and become champions for accountable care adoption in their industry/region or nationally.
Interactive Measurement Tracks
This interactive tool provides illustrative examples of capabilities organizations might pursue in their efforts to advance along the Accountable Care Curve. Organizations do not necessarily need to pursue all of these capabilities to realize a certain stage of accountable care.
Payment Reform Capability Examples
LEGEND: ![]() Purchaser |
Purchaser | ![]() Provider |
Provider | ![]() Payer
Payer
Click on any of the Transformation Stages, sub-headings, and capabilities below to learn more!
- Manage financial reconciliation



- Leveraging multiple reports (integrated clinical, claims, quality, and financial data)



- Development of contract management platform


- Integrated financial and clinical team actively engaged to incorporate clinical perspectives with data outputs to identify insights and target performance improvement opportunities

- Network performance and reporting management

- Financial incentive alignment across organizational leadership and providers focused on accountable care



- Continuous improvement outputs based on insights and target performance



- Enhanced reporting of delegated and collaborative community services on member patient outcomes and plan/provider performance


Quality Capability Examples
LEGEND: ![]() Purchaser |
Purchaser | ![]() Provider |
Provider | ![]() Payer
Payer
Click on any of the Transformation Stages, sub-headings, and capabilities below to learn more!
- Engage and collaborate with provider leadership in reconciling perceived conflicts between clinical quality and governmental and health plan performance quality metrics



- Develop key performance indicator management and alignment



- Provide transparent quality benchmarking methodology



- Incorporation of patient-reported outcomes into performance reporting



- Aggregate quality reporting incorporating utilization, sites of service, and patient outcomes


- Encourage provider-specific reporting incorporating quality, utilization, financial outcomes, and benchmark comparisons


Data and Infrastructure Capability Examples
LEGEND: ![]() Purchaser |
Purchaser | ![]() Provider |
Provider | ![]() Payer
Payer
Click on any of the Transformation Stages, sub-headings, and capabilities below to learn more!
- Develop quality, outcomes, financial, and utilization reporting



- Leverage employer and administrative services only (ASO) reporting



- Comparative and benchmarked performance reporting across all alternative payment model contracts



- Analytics rules engine with multidimensional identification and stratification modeling


- Create chronic disease registries with electronic health records (EHR) and claims-based data


Multi-stakeholder Alignment and Design Capability Examples
LEGEND: ![]() Purchaser |
Purchaser | ![]() Provider |
Provider | ![]() Payer
Payer
Click on any of the Transformation Stages, sub-headings, and capabilities below to learn more!
- Build qualitative indicators for multi-stakeholder network success



- Development of aligned measurement sets



- Create appropriate partnerships and initiatives to address the needs of historically underserved populations with complex needs



- Implement interoperable data exchange/electronic clinical quality measures


Payment Reform Capability Examples
LEGEND: ![]() Purchaser |
Purchaser | ![]() Provider |
Provider | ![]() Payer
Payer
Click on any of the Transformation Stages, sub-headings, and capabilities below to learn more!
- Manage financial reconciliation



- Leveraging multiple reports (integrated clinical, claims, quality, and financial data)



- Development of contract management platform


- Integrated financial and clinical team actively engaged to incorporate clinical perspectives with data outputs to identify insights and target performance improvement opportunities

- Network performance and reporting management.

- Financial incentive alignment across organizational leadership and providers focused on accountable care



- Continuous improvement outputs based on insights and target performance



- Enhanced reporting of delegated and collaborative community services on member patient outcomes and plan/provider performance


Quality Capability Examples
LEGEND: ![]() Purchaser |
Purchaser | ![]() Provider |
Provider | ![]() Payer
Payer
Click on any of the Transformation Stages, sub-headings, and capabilities below to learn more!
- Engage and collaborate with provider leadership in reconciling perceived conflicts between clinical quality and governmental and health plan performance quality metrics



- Develop key performance indicator management and alignment



- Provide transparent quality benchmarking methodology



- Incorporation of patient-reported outcomes into performance reporting



- Aggregate quality reporting incorporating utilization, sites of service, and patient outcomes


- Encourage provider-specific reporting incorporating quality, utilization, financial outcomes, and benchmark comparisons


Data and Infrastructure Capability Examples
LEGEND: ![]() Purchaser |
Purchaser | ![]() Provider |
Provider | ![]() Payer
Payer
Click on any of the Transformation Stages, sub-headings, and capabilities below to learn more!
- Develop quality, outcomes, financial, and utilization reporting



- Leverage employer and administrative services only (ASO) reporting



- Comparative and benchmarked performance reporting across all alternative payment model contracts



- Analytics rules engine with multidimensional identification and stratification modeling


- Create chronic disease registries with electronic health records (EHR) and claims-based data


Multi-stakeholder Alignment and Design Capability Examples
LEGEND: ![]() Purchaser |
Purchaser | ![]() Provider |
Provider | ![]() Payer
Payer
Click on any of the Transformation Stages, sub-headings, and capabilities below to learn more!
- Build qualitative indicators for multi-stakeholder network success



- Development of aligned measurement sets



- Create appropriate partnerships and initiatives to address the needs of historically underserved populations with complex needs



- Implement interoperable data exchange/electronic clinical quality measures


Health Equity Advancements Capability Examples
LEGEND: ![]() Purchaser |
Purchaser | ![]() Provider |
Provider | ![]() Payer
Payer
Click on any of the Transformation Stages, sub-headings, and capabilities below to learn more!
Submit your feedback, examples, and key resources to the HCPLAN at HCPLAN@deloitte.com
















 Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models.
Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models. Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System.
Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System. Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.
Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.


 Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.
Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.





