HCPLAN Reaffirms Commitment to Value-Based Care
MAY 19, 2025
May 19, 2025 — Value-based care remains fundamental to the mission and strategy of the Health Care Payment Learning & Action Network (HCPLAN). The HCPLAN will resume its longstanding efforts to improve health care quality and outcomes while reducing health care costs through alternative payment models (APMs). In the coming months, the HCPLAN will launch four new initiatives focused on health care choice and competition, patient empowerment, preventative care, and technology-enabled health care. These initiatives align with the new Center for Medicare and Medicaid Innovation (CMMI) strategy to “Make America Healthy Again” and underscore the crucial role of public-private partnerships in accelerating innovation and driving positive change in these focus areas.
“Public-private collaboration is needed now more than ever to leverage the innovation that is happening in the private sector and align this work with public policy to drive meaningful change in health care,” said Dr. Mark McClellan, co-chair of the HCPLAN and Director of the Duke-Margolis Institute for Health Policy.
“The HCPLAN will bring together a wide range of perspectives and experience to find practical steps to empower people, keep Americans healthy, and drive out unnecessary costs,” said Abe Sutton, CMMI Director. “CMS will benefit from this focused collaboration to inform our work, and we expect that states, employers, and health plans will be able to take more effective action to support their beneficiaries as well.”
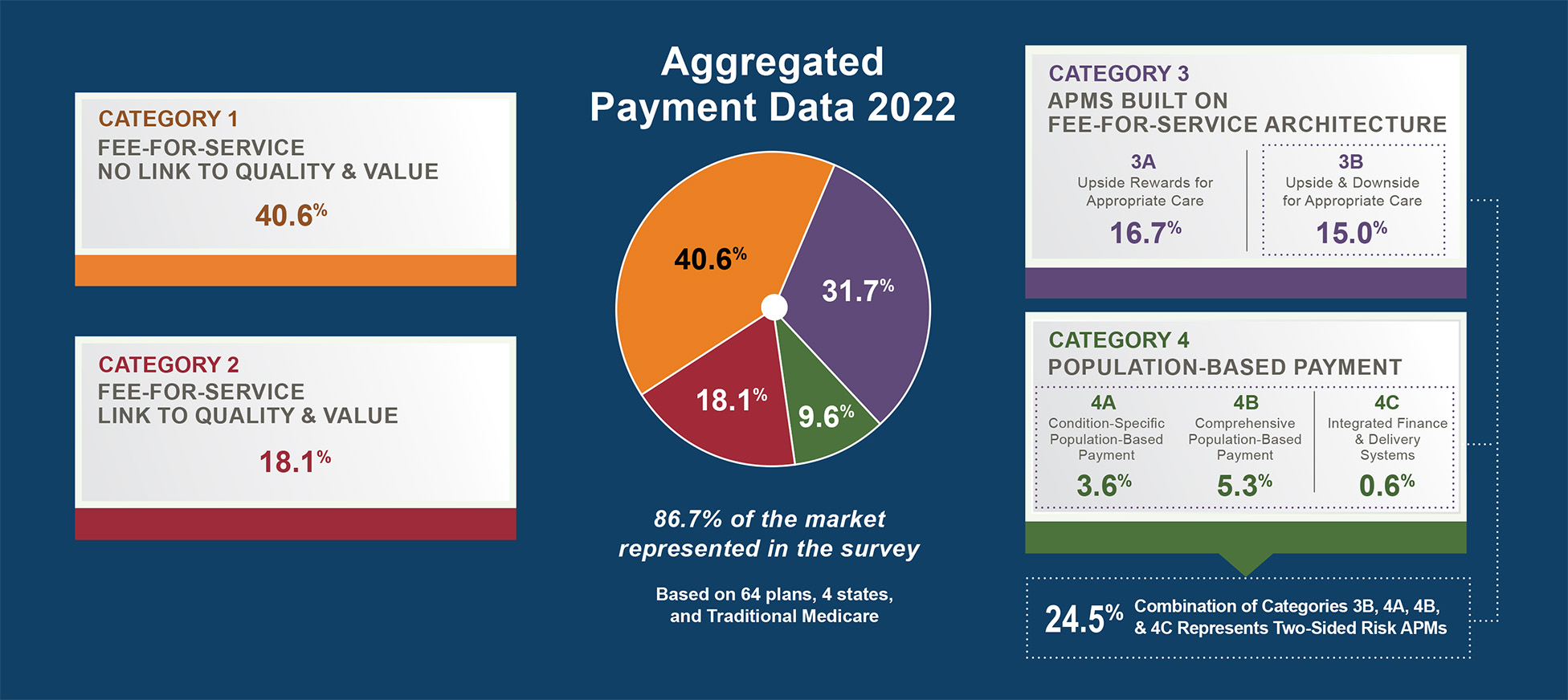
With this shift in initiatives to advance value-based care and improve health care quality for Americans, the HCPLAN will discontinue its CMMI-funded APM Measurement Effort. “The HCPLAN sees this as an opportunity to focus our actions at the state and federal level to achieve meaningful progress on value-based care,” said Dr. Judy Zerzan-Thul, HCPLAN co-chair and Chief Medical Officer at Washington State Healthcare Authority. Since its launch in 2015, the HCPLAN APM Measurement Effort has monitored the shift of U.S. health care from fee-for-service to APMs. The 2024 APM Measurement Effort results demonstrated the continued growth in APM adoption and initiatives to enhance patient access, affordability, and quality of care. As part of its efforts to advance the availability and reduce the cost of key data needed to improve care, the HCPLAN will explore alternative pathways for the continuation of this effort.
“We look forward to action based on this shared commitment to make progress in Medicaid and throughout our health care system, centering prevention and strong primary care to improve health for all Americans,” said Dr. Alice Chen, HCPLAN co-chair and Chief Health Officer at Centene.
Additional information on HCPLAN priorities and initiatives is forthcoming. In the meantime, inquiries may be directed to hcplan@deloitte.com.
About the HCPLAN
The Health Care Payment Learning & Action Network (HCPLAN) is an active group of public and private health care leaders providing thought leadership, strategic direction, and support to accelerate our health care system’s adoption of alternative payment models (APMs). The HCPLAN mobilizes payers, providers, purchasers, patients, product manufacturers, policymakers, and other stakeholders in a shared mission to innovate health care, increase choice and competition, empower patients, reduce barriers to APM participation, and promote shared accountability. The HCPLAN also serves as a trusted convener to connect the public and private sectors in order to identify, share, and scale promising practices that improve health.















 Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models.
Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models. Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System.
Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System. Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.
Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.


 Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.
Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.





