As debate rages around payment models, many questions arise, such as: Who are we working to serve and how do we involve them? What does the best evidence suggest will make a difference in health and well-being? How do we maximize the health benefits that come from every dollar the American people spend for their care? The payment model debates are intense, they are passionate, and they shift as evidence and community expectations evolve. Since the founding of Kaiser Permanente 70 years ago, its people have been asking themselves these important questions. To help find answers, patients and their families are now partnering with us, co-creating health through care and support that best meets the patient’s goals, needs, and expectations.
At Kaiser Permanente, the search for answers reflects a relentless effort to support the goals our members have for their own health. Throughout our own intense debates, one thing stands certain; the discussion is not about high-margin therapies or maximizing revenue, but about doing what’s right for the patient at a price that is in reach for those we serve.
Pioneering Population-Based Payments
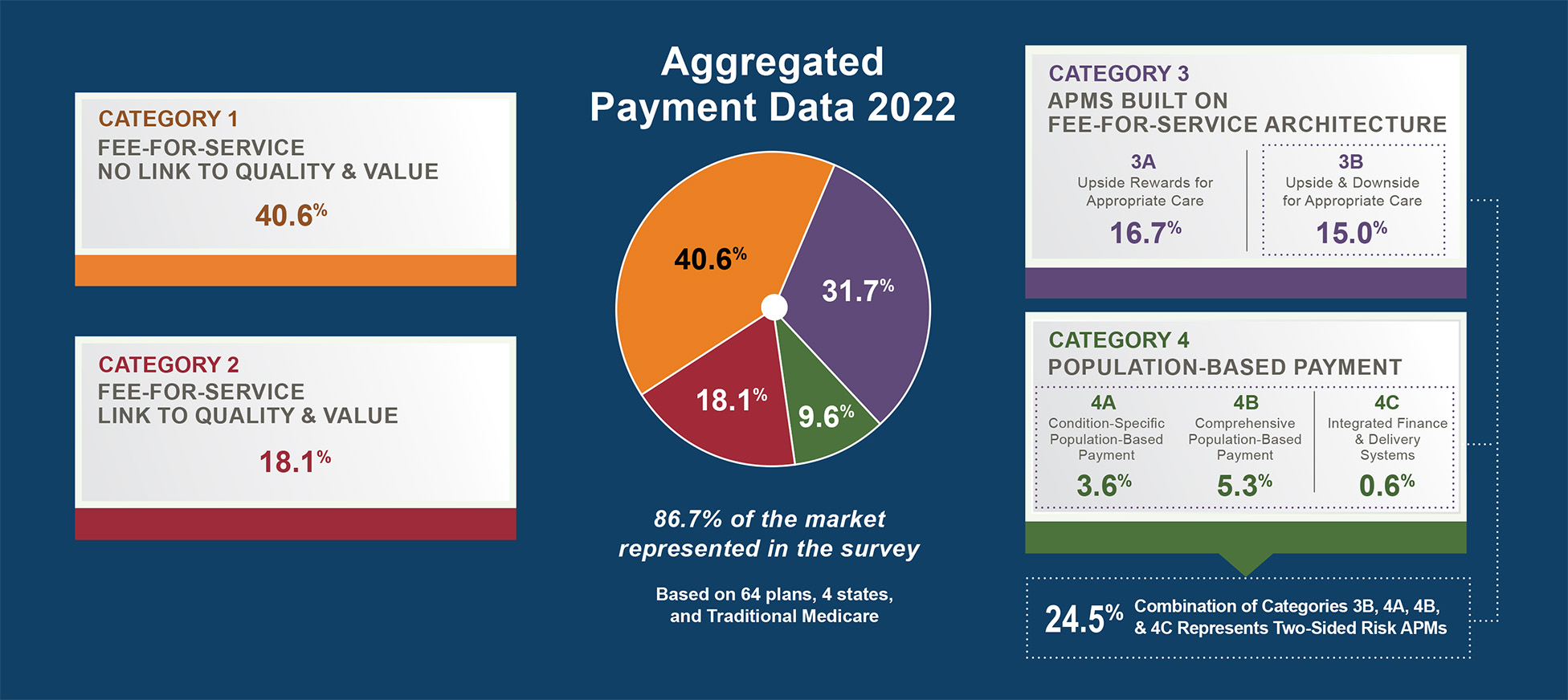
In drafting the Alternative Payment Model (APM) Framework White Paper, the Health Care Payment Learning and Action Network (LAN) set out to describe the current landscape of models used to finance health care, from full fee-for-service (Category 1) through full population-based payment (Category 4). The paper shows that the fee-for-service model still dominates, and proposes that a shift in the direction of population-based payment would result in more patient-centered care.
Wisely, the framework suggests that a shift along the continuum between these two will occur as the industry evolves. The expectation is that purchasers, both entities and individuals, will move to systems that prove they can serve the patient well, and do so at an affordable cost. In other words, those systems that consumers choose most often will be those that can dramatically increase health through care and other services, while keeping the price affordable. The premise is that payment methods that reward value will win.
Kaiser Permanente’s highly integrated financing and delivery model sits in Category 4 of the APM Framework. As a leader and innovative pioneer with over 70 years of experience, we can attest to the durability of the model.
A Tradition of Relationships and Rewards
Kaiser Permanente was born out of the challenge of providing Americans with medical care during the Great Depression and World War II, when most people could not afford to go to a doctor.
Kaiser Permanente applied multiple innovative ideas during those early years. Prepaid insurance spread the cost to make it more affordable. Physicians in group medical practice maximized their abilities to care for patients. They began to focus as much on preventing illness as on caring for the sick.
That foundation has allowed us, from day one, to incentivize our physicians and care teams to focus on maximizing the health of their patients through a long term relationship, rather than rewarding them for the volume of services they perform. Our philosophy, structure, and incentives are aligned and enable our physicians, nurses, and staff to work collaboratively and create a culture of healing. We inspire good health and provide the best treatments and personalized care that our members need to get, and stay, healthy.
One prime example of the health benefits that can occur within a model that incentivizes the best interest of the health of the patient is in our work around cardiac care for those patients with diabetes. By partnering closely with our population of diabetic patients at risk for heart attack and stroke, we developed the ALL (Aspirin, Lisinopril and Lipid-lowering medication) protocol. ALL research has shown that when taken together once a day, this trio of low-cost, low-risk medicines lowered the incidence of heart attacks and stroke in this population of patients by more than 60 percent.
In 2014, Kaiser Permanente had achieved nearly 95 percent hypertension control rates across the regions we serve, far above the national average of 52 percent.
What would that mean for everyone else? If the rest of the U.S. managed the blood pressure of hypertensive patients as well as Kaiser Permanente does, many thousands of heart attacks and strokes could be prevented each year, and several hundred thousand deaths could be prevented over 10 years.
Value-Based Payments: a Rich Past, a Promising Future
For 25 years, stone by stone, the health care quality movement has built the foundation for value-based payment. This foundation was not in place in our country in the 1990s, when population-based payment brought hope that the industry could meet the cost challenge in health care. Without a strong quality story to tell, population-based payment fell from favor in most places. Times have changed. The health care quality movement continues to grow and improve, and it is now shifting to a more outcome-oriented approach. That approach will only strengthen the case that we make to the country about the value of what we do. Most importantly, as Kaiser Permanente and other organizations have learned over many decades, the way we pay for care changes the nature of the debates we have. It also changes the way we act as we seek to serve our members and our communities in the most valuable way possible. It frees us to partner with them in a different way, with a dedicated focus on the value of what we do to co-create health now and in the future.
Please note that guest blogs from Guiding Committee and Work Group members represent the views of the individual authors and do not represent official positions of the Guiding Committee, Work Groups, CAMH, or CMS.















 Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models.
Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models. Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System.
Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System. Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.
Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.


 Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.
Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.





