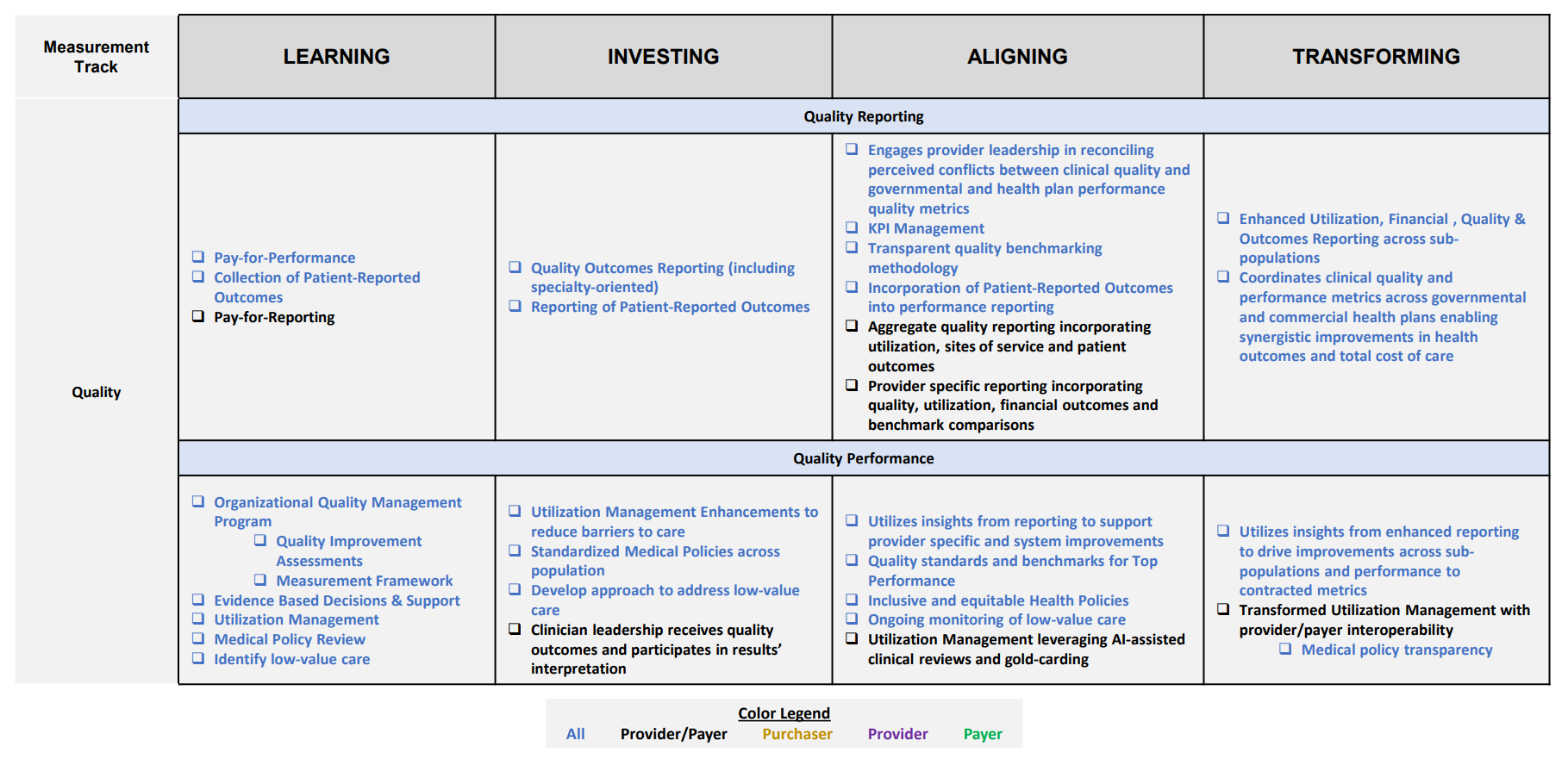
Learning Stage
Supports understanding of standard quality metrics and current state of quality performance
Investing Stage
Supports establishing evidence-based quality goals with ongoing data collection for measuring improvement and progress towards goals
Aligning Stage
Supports benchmarking quality performance results and executing improved outcomes towards person-centered care
Transforming Stage
Supports using standardized system-wide processes to predict rising risk within populations to improve patient experience and drive high-quality care for all
Pay-for-Performance
Developing an incentive structure to demonstrate successful achievement of defined process and clinical measures to earn shared savings and/or incentive payments
Collection of Patient-Reported Outcomes (PRO)
Report of the status of a patient’s health conditions that comes directly from the patient, without interpretation of the patient’s response by a clinician or anyone else; examples of patient self-reported data collection tools include Patient-Reported Outcomes Measurement Information System (PROMIS), Medicare Health Outcomes Survey, FOTO Patient Outcomes
Pay-for-Reporting
Developing an incentive structure to demonstrate successful achievement of defined process and clinical measures to earn shared savings and/or incentive payments
Quality Outcomes Reporting (including specialty-oriented)
Integration with Data/Infrastructure measurement track for Enterprise Data Warehouse. Includes establishing the importance of data quality in driving business decisions
Reporting of Patient-Reported Outcomes
Effective collection and analysis of patient-reported outcomes; timely collection and use of alternative collection methods (e.g., mobile devices)
Engages provider leadership in reconciling perceived conflicts between clinical quality and governmental and health plan performance quality metrics
Ensuring that provider/clinical stakeholders are included in quality reporting analysis and resolving potential conflicts early in the performance review period
KPI Management
Aligning on what key performance indicators the organization will focus on as well as tools to monitor results with actionable interventions
Transparent quality benchmarking methodology
Methodology must be adjusted for population mix, risk (including social determinants of health) and market. Also includes participation in clinical registries
Incorporation of Patient-Reported Outcomes into performance reporting
Measure developers should construct quality measures that apply the outcome data collected by the tools to measure the quality of care
Aggregate quality reporting incorporating utilization, sites of service and patient outcomes
Inclusion of multiple sources and types of quality data for well-rounded measurement
Provider specific reporting incorporating quality, utilization, financial outcomes, and benchmark comparisons
Ensuring that quality reporting includes multiple sources of measurement and comprehensive assessment within a defined provider network/group
Enhanced Utilization, Financial, Quality & Outcomes Reporting across sub-populations
Aggregated from multiple populations/subpopulations to identify multi-dimensional opportunities
Coordinates clinical quality and performance metrics across governmental and commercial health plans enabling synergistic improvements in health outcomes and total cost of care
Application of best practices and efficiencies identified from individual payer arrangements across all contracts
Quality Reporting
Supports capturing and benchmarking quality reporting metrics across populations to track total cost of care
Quality Performance
Emphasize ongoing quality monitoring and governance to drive support around quality-driven decision making
Organizational Quality Management Program
Standardize processes and structure to reduce variation, achieve predictable results, and improve outcomes for patients, healthcare systems, and organizations. Structures may include technology, culture, and leadership
Quality Improvement Assessments
Processes that include testing acceptance/adherence to new/revised practices, determining how the new practices are affecting the delivery of patient-centered care, assessment of how much patient care is improving
Measurement Framework
Understanding the organizational approach/framework on quality measurement that will be used for consistent monitoring and comparison year over year
Evidence Based Decisions & Support
Understanding the value and purpose of effective decision making by leveraging data analysis and information. Putting support systems in place to ensure compliance and inter-rater reliability
Utilization Management
Framework to evaluate medical necessity, appropriateness and efficiency of health care services, procedures, and facilities
Medical Policy Review
Collection and clinical review of medical records and related information for specific conditions/procedures against predefined guidelines and requirements
Identify low-value care
Services that provide little or no benefit to patients, have potential to cause harm, incur unnecessary costs to patients, or waste limited healthcare resources; data-driven process
Utilization Management Enhancements to reduce barriers to care
Includes re-evaluation of prior authorization list to eliminate low value/non-standard sub-categories and electronic submissions
Standardized Medical Policies across population
Configuration of medical policies guidelines to be applicable for entire population instead of specific sub-populations; eases burden on providers to determine applicability of medical policies for specific patient types
Develop approach to address low-value care
Approach may include focus on appropriateness of care that is anchored in improving outcomes (high-value care)
Clinician leadership receives quality outcomes and participates in results’ interpretation
Ensuring clinical stakeholders participate in outcomes discussions to determine interventions and next steps
Utilizes insights from reporting to support provider specific and system improvements
Application of quality performance results to drive provider specific process improvements
Quality standards and benchmarks for top performance
Using top performance benchmarks and quality standards to align quality improvement plan targets
Inclusive and equitable Health Policies
Includes comparison against industry standards and best practices
Ongoing monitoring of low-value care
Incorporating low-value care monitoring and analysis into ongoing quality performance reviews
Utilization Management leveraging AI-assisted clinical reviews and gold-carding
Increased clinical review efficiency and accuracy to reduce administrative burden
Utilizes insights from enhanced reporting to drive improvements across sub-populations and performance to contracted metrics
Application of quality performance results to drive larger scale process improvements that influence larger populations and drive improvements with contracted metrics
Transformed Utilization Management with provider/payer interoperability
Includes implementation of FHIR API standards


















 Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models.
Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models. Mr. James Sinkoff is the Deputy Executive Officer and Chief Financial Officer for Sun River Health (formerly known as Hudson River HealthCare), and the Chief Executive Officer of Solutions 4 Community Health (S4CH); an MSO serving FQHCs and private physician practices.
Mr. James Sinkoff is the Deputy Executive Officer and Chief Financial Officer for Sun River Health (formerly known as Hudson River HealthCare), and the Chief Executive Officer of Solutions 4 Community Health (S4CH); an MSO serving FQHCs and private physician practices. Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System.
Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System. Dr. Brandon G. Wilson, DrPH, MHA (he, him, his) joined Community Catalyst as the Director of the Center for Consumer Engagement in Health Innovation, where he leads the Center in bringing the community’s experience to the forefront of health systems transformation and health reform efforts, in order to deliver better care, better value and better health for every community, particularly vulnerable and historically underserved populations. The Center works directly with community advocates around the country to increase the skills and power they have to establish an effective voice at all levels of the health care system. The Center collaborates with innovative health plans, hospitals and providers to incorporate communities and their lived experience into the design of systems of care. The Center also works with state and federal policymakers to spur change that makes the health system more responsive to communities. And it provides consulting services to health plans, provider groups and other health care organizations to help them create meaningful structures for engagement with their communities.
Dr. Brandon G. Wilson, DrPH, MHA (he, him, his) joined Community Catalyst as the Director of the Center for Consumer Engagement in Health Innovation, where he leads the Center in bringing the community’s experience to the forefront of health systems transformation and health reform efforts, in order to deliver better care, better value and better health for every community, particularly vulnerable and historically underserved populations. The Center works directly with community advocates around the country to increase the skills and power they have to establish an effective voice at all levels of the health care system. The Center collaborates with innovative health plans, hospitals and providers to incorporate communities and their lived experience into the design of systems of care. The Center also works with state and federal policymakers to spur change that makes the health system more responsive to communities. And it provides consulting services to health plans, provider groups and other health care organizations to help them create meaningful structures for engagement with their communities. Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.
Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.


 Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.
Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.








