The 2024 HCPLAN Summit, held in Baltimore on November 14, brought together a record-breaking number of health care professionals, thought leaders, and policy advocates to advance accountable care and value-based payment models. The event included dynamic sessions on critical topics like health equity, multi-payer alignment, and enhancing patient experience. Leaders from the Centers for Medicare & Medicaid Services (CMS) shared insights into improving care for underserved populations and tackling measurement gaps, while the unveiling of the 2024 Measurement Effort results showcased nationwide progress in payment reform. The HCPLAN Summit provided a unique platform for collaboration, learning, and driving meaningful change in health care.
Did you miss some of the 2024 HCPLAN Summit sessions? Are you looking to revisit key moments? Recordings from most sessions are now available! Watch the full videos on the HCPLAN Summit website.
 Transforming Health Care: A Fireside Chat with CMS and HCPLAN Leadership
Transforming Health Care: A Fireside Chat with CMS and HCPLAN Leadership
The HCPLAN Summit’s fireside chat inspired attendees with a bold vision for value-based, quality-driven health care.
Dr. Mark McClellan, Dr. Alice Hm Chen, and Jonathan Blum tackled key issues like workforce challenges, specialty care, and value-based care partnerships, guided by moderator Kate Davidson.
- Kate Davidson highlighted the HCPLAN’s progress in advancing value-based care and tackling barriers like administrative burden and infrastructure challenges, while emphasizing payment models that prioritize affordability, access, and patient experience.
- Dr. Mark McClellan highlighted the importance of multi-stakeholder collaboration for value-based care adoption, focusing on shared accountability among payers, providers, and patients, and strategies for aligning incentives to improve outcomes and equity.
- Dr. Alice Hm Chen stressed the widespread adoption of value-based payment models in Medicaid, noting the shift to comprehensive care for vulnerable populations and the need for standardized definitions to align on meaningful outcomes.
- Jonathan Blum shared CMS’s progress toward its 2030 goals of 100 percent accountable care relationships for Medicare and 50 percent accountable care relationships for Medicaid, highlighting strides in unified measures, simplified models, and system-wide collaboration for transformation.
 CMS’s Approach to Multi-Payer Engagement and Delivery System Reform
CMS’s Approach to Multi-Payer Engagement and Delivery System Reform
A powerhouse panel of CMS leaders delved into the agency’s efforts to align Medicare, Medicaid, and private payers in pursuit of meaningful delivery system reform.
Featuring Dr. Meena Seshamani, Daniel Tsai, Dr. Dora Hughes, and moderator Liz Fowler, the session highlighted critical advancements and strategies shaping value-based care across CMS programs.
- Liz Fowler described the HCPLAN’s achievements, including defining accountable care, broadening membership, and progressing toward universal accountable care in Medicare and Medicaid.
- Dr. Dora Hughes outlined the work of the Center for Clinical Standards & Quality on embedding equity in quality reporting, which includes mandatory screenings in quality programs, targeting maternal health and organ transplantation for underserved groups, and strengthening nursing home staffing requirements.
- Daniel Tsai spoke about integrating disparity reporting into Medicaid to focus on race and ethnicity, aiming to streamline coverage and reduce barriers for underserved populations.
- Dr. Meena Seshamani praised CMS’s collaborative efforts and how pilot programs have expanded to Medicare, Medicaid, and CHIP, highlighting the scaling of the ACO Investment Model and the integration of health equity benchmarks into the Medicare Shared Savings Program.
Rural Health and APMs: Reaching New Frontiers

Every year, the HCPLAN conducts a national effort to assess the adoption of APMs over time and track progress towards the HCPLAN’s goals. Payment data is reported by line of business (LOB) — Commercial, Medicaid, Medicare Advantage, and Traditional Medicare.
Highlights from the 2024 Measurement Effort results include:
- Two-sided risk APM spending (where providers share savings and losses with payers) increased across every line of business in 2023.
- Ninety-six percent of respondents believe APM adoption will result in better quality care.
- Eighty-eight percent of respondents believe APM adoption will result in more affordable care.
- Every strategy to address health-related social needs and improve health equity through provider incentives increased from 2022 to 2023, and four of the top five strategies increased by double-digit percentage points.
- Traditional Medicare increased the number of beneficiaries in an accountable care arrangement and is now nearly halfway to its 2030 goal.
HCPLAN Measurement Results
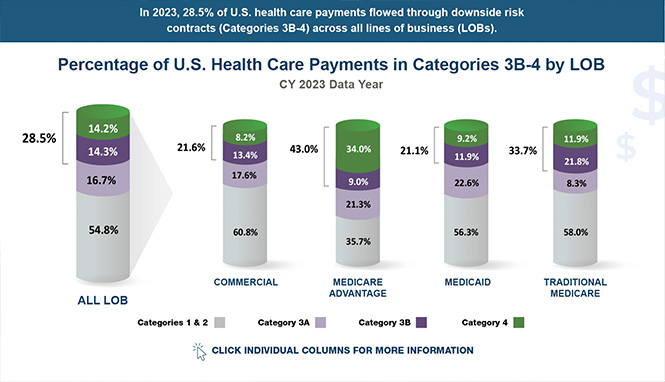
Every year, the HCPLAN conducts a national effort to assess the adoption of APMs over time and track progress towards the HCPLAN’s goals. Payment data is reported by line of business (LOB) — Commercial, Medicaid, Medicare Advantage, and Traditional Medicare.
Highlights from the 2024 Measurement Effort results include:
- Two-sided risk APM spending (where providers share savings and losses with payers) increased across every line of business in 2023.
- Ninety-six percent of respondents believe APM adoption will result in better quality care.
- Eighty-eight percent of respondents believe APM adoption will result in more affordable care.
- Every strategy to address health-related social needs and improve health equity through provider incentives increased from 2022 to 2023, and four of the top five strategies increased by double-digit percentage points.
- Traditional Medicare increased the number of beneficiaries in an accountable care arrangement and is now nearly halfway to its 2030 goal.
Person Perspectives Council Guidance Document

A person-centered or whole-person care system ensures that health care professionals treat patients holistically, addressing their overall health rather than focusing on isolated symptoms, to improve health outcomes.
The Person Perspectives Council amplifies the voices of organizations representing individuals, patients, and caregivers. This council has developed the guidance document “Understanding People’s Health Care Priorities,” designed to help health plans and providers understand and prioritize what people value most in their health care.
The findings highlight what people prioritize in health care based on their unique experiences, personal needs, and community context. These priorities vary depending on the individual and their family’s interactions with the health care system over time. They fall into three key areas — affordability, experience, and access — that reflect common concerns and foundational needs that are often overlooked. These priorities are not an exhaustive list or fixed framework. Instead, they represent what matters most to people in today’s health care environment. Additionally, these areas often overlap and influence one another.
Alignment Landscape
The Alignment Landscape offers a comprehensive overview of strategies and resources designed to enhance collaboration across the health care industry.
Alignment builds a sustainable foundation for system-wide transformation by reducing the administrative burden placed on health plans, providers, purchasers, and community organizations who must contend with multiple value-based care arrangements. By promoting alignment on a national and cross-state level, it helps streamline efforts and expand engagement in value-based care initiatives.
Users of the Alignment Landscape can explore tailored insights, like how providers can prepare for data-sharing rules or how community organizations can partner with health plans.
Filters can be used to access guidance on regulations, initiatives, partnerships, and policies to advance value-based care.
HEAT Social Return on Investment Document
The Health Equity Advisory Team’s new document on social return on investment (social ROI) is a follow-up to its 2023 guidance document on partnering with community-based organizations, and highlights the importance of investing in programs that deliver measurable benefits beyond traditional metrics.
Social ROI is a framework for measuring and accounting for the broad social value of programs relative to the resources invested. The outcomes are comprehensive and diverse, including improved employment and academic performance, reduced food insecurity, reduced truancy rates, environmental benefits, and increased well-being.
This guidance offers a comprehensive framework for evaluating the social, economic, and environmental value of health care programs, fostering a more equitable and healthier future. It addresses current challenges in measuring social ROI in health care, and highlights promising practices to support payers, purchasers, employers, health plans, and health care delivery organizations in integrating the social ROI framework into decision-making processes.
Accountable Care Action Collaborative Guidance Document
The Accountable Care Action Collaborative’s new document “Advancing Health Equity Through APMs” offers guidance for creating alternative payment models (APMs) that promote health equity. It emphasizes the critical role of demographic and social data collection in identifying health disparities and improving care coordination. Drawing from real-world observations and promising multi-sector practices, this document outlines practical steps to operationalize accountable care initiatives that explicitly integrate incentives for health equity.
Explore how organizations have used the following building blocks to advance health equity as part of their accountable care initiatives with short- and long-term promising practices:
- Leadership & Organizational Commitment
- Data Collection & Sharing
- Payment Alignment
- Care Delivery
- Oversight & Performance Management
HCPLAN News
Measurement Effort
- Summarizing our 2024 Measurement Effort data, this article shares how health plans are increasing their use of value-based payment models to drive higher-quality and more affordable care. Significant growth has been noted in both Medicare Advantage and commercial markets over recent years.
Value-Based Models Picked Up Steam in 2023: 5 Numbers To Know
- This article highlights the fact that 2023 saw significant growth in value-based care models, with major health insurers increasing their investments in these arrangements to enhance patient outcomes and contain costs.
HCPLAN Survey Data Finds Progress on Alternative Payment Models
- This article describes progress towards APM adoption from our Measurement Effort data, citing that, from 2022 to 2023, value-based arrangements across various sectors increased from 41.3 percent to 45.2 percent.
Healthcare IT Today Bonus Feature – November 17, 2024
- A statistic from our 2024 Measurement Effort data was included in a weekly bonus feature article, stating that “29% of health care payments in 2023 involved downside risk arrangements.”
Accountable Care Organizations
- Referencing data from the 2024 HCPLAN Summit, this article emphasizes CMS’s commitment to advancing value-based care in nursing homes, highlighting efforts to overcome current challenges related to care coordination and financial risks.
Notable Quotes
Top CMS Official Urges Trump Administration to Treat Medicaid With Care
- In this article in Healthcare Dive, Director of the Center for Medicaid and CHIP Services Daniel Tsai’s powerful message from the 2024 HCPLAN Summit was highlighted: “Treat the program the way you would want it if you, your kids, your family, your closest friends, relied on the Medicaid and CHIP program.”
Looking Ahead
Next year marks the 10-year anniversary of the HCPLAN! We cannot wait to celebrate a decade of progress in health care payment reform in 2025. This milestone year will bring together leaders and visionaries to reflect, share insights, and drive forward innovation for improved quality in patient care. With a decade of impactful conversations and achievements, next year promises to be an occasion to remember!
Our Vision
Improved and equitable health outcomes, resulting in overall lower total cost of care.
Our Mission
The HCPLAN will advance multi-stakeholder payment reforms to enable coordinated health care that achieves better health, equity, and affordability.
Our Goal Statement
Accelerate the percentage of U.S. health care payments tied to quality and value in each market segment through the adoption of two-sided risk alternative payment models (Categories 3B and 4 of the HCPLAN APM Framework).


















 Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models.
Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models. Mr. James Sinkoff is the Deputy Executive Officer and Chief Financial Officer for Sun River Health (formerly known as Hudson River HealthCare), and the Chief Executive Officer of Solutions 4 Community Health (S4CH); an MSO serving FQHCs and private physician practices.
Mr. James Sinkoff is the Deputy Executive Officer and Chief Financial Officer for Sun River Health (formerly known as Hudson River HealthCare), and the Chief Executive Officer of Solutions 4 Community Health (S4CH); an MSO serving FQHCs and private physician practices. Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System.
Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System. Dr. Brandon G. Wilson, DrPH, MHA (he, him, his) joined Community Catalyst as the Director of the Center for Consumer Engagement in Health Innovation, where he leads the Center in bringing the community’s experience to the forefront of health systems transformation and health reform efforts, in order to deliver better care, better value and better health for every community, particularly vulnerable and historically underserved populations. The Center works directly with community advocates around the country to increase the skills and power they have to establish an effective voice at all levels of the health care system. The Center collaborates with innovative health plans, hospitals and providers to incorporate communities and their lived experience into the design of systems of care. The Center also works with state and federal policymakers to spur change that makes the health system more responsive to communities. And it provides consulting services to health plans, provider groups and other health care organizations to help them create meaningful structures for engagement with their communities.
Dr. Brandon G. Wilson, DrPH, MHA (he, him, his) joined Community Catalyst as the Director of the Center for Consumer Engagement in Health Innovation, where he leads the Center in bringing the community’s experience to the forefront of health systems transformation and health reform efforts, in order to deliver better care, better value and better health for every community, particularly vulnerable and historically underserved populations. The Center works directly with community advocates around the country to increase the skills and power they have to establish an effective voice at all levels of the health care system. The Center collaborates with innovative health plans, hospitals and providers to incorporate communities and their lived experience into the design of systems of care. The Center also works with state and federal policymakers to spur change that makes the health system more responsive to communities. And it provides consulting services to health plans, provider groups and other health care organizations to help them create meaningful structures for engagement with their communities. Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.
Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.


 Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.
Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.








