
The Accountable Health Care: Outcomes from the Field session featured leaders and experts across the health care industry, including:

Panelists shared their firsthand experiences with alternative payment model adoption and accountable care relationships and success stories of value-based care positively impacting patients and providers. The discussion highlighted key points such as serving rural areas in value-based care arrangements, prioritizing coordination across the continuum of care, and accelerating value-based care arrangements in specialty areas of care.
If you missed this dynamic conversation, check out the recording and catch up on the work being done to advance alternative payment model adoption.

 Health care providers and safety-net organizations serve populations that are facing growing risks from climate change. By reducing the environmental impact of health care operations, providers can further contribute to the overall well-being of their communities. To help providers reduce the negative impact on the environment, the U.S. Department of Health & Human Services (HHS) Office of Climate Change and Health Equity (OCCHE) recently launched its Catalytic Program utilizing the Inflation Reduction Act.
Health care providers and safety-net organizations serve populations that are facing growing risks from climate change. By reducing the environmental impact of health care operations, providers can further contribute to the overall well-being of their communities. To help providers reduce the negative impact on the environment, the U.S. Department of Health & Human Services (HHS) Office of Climate Change and Health Equity (OCCHE) recently launched its Catalytic Program utilizing the Inflation Reduction Act.
Join HCPLAN and OCCHE on May 8 from 2:30-3:30 PM ET to learn how environmental stewardship and value-based care are interdependent.
OCCHE Health Sector Lead Joe McCannon will share information about tax credit and grant-supported opportunities for health care providers to invest in clean energy through the Catalytic Program and the Inflation Reduction Act.
This collaborative event will also feature a panel of health professionals from value-based health care organizations that are simultaneously fighting climate change, reducing health care costs, and improving health outcomes in their communities. More information coming soon!

Welcome Dan Liljenquist and Deepak Sadagopan to the Executive Forum!
- Dan Liljenquist serves as the chief strategy officer at Intermountain Health, a health care system committed to helping people live their healthiest lives possible through quality, sustainable, and affordable care. From cutting-edge research to groundbreaking clinical studies, Intermountain Health is advancing in every aspect of health care delivery to create more equitable experiences for all. Dan plays a key role in driving Intermountain Health’s organizational priorities of clinical excellence, serving patients with compassion and respect, and building community through teamwork and belonging.
- Deepak Sadagopan serves as the chief operating officer of population health at Providence, an organization committed to reducing health disparities through personal and institutional work to enable every patient and the communities they serve a chance to live their healthiest life. Deepak reinforces this vision as a champion of value-based care and Health IT policy initiatives that can enable equitable access to health care. He works closely with payers and providers in the use of technology to drive business decisions making the transition from volume to value-based delivery models.
Learn more about the Executive Forum.

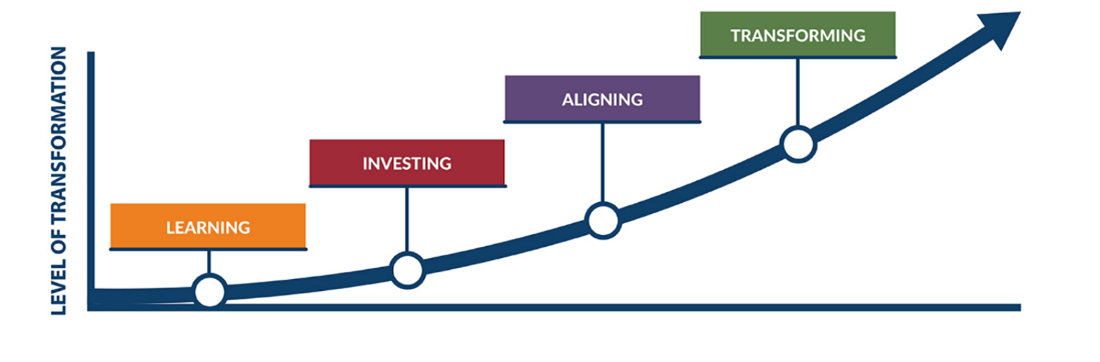
Take this brief five-question survey to help HCPLAN understand where you are on the curve and how the curve is supporting your journey.

Press Play: The Leapfrog Group President & CEO and HCPLAN Accountable Care Action Collaborative (ACAC) Co-Chair Leah Binder makes a guest appearance on Business Group on Health podcast
Listen: The Power of Transparency to Transform Patient Safety | Business Group on Health (businessgrouphealth.org)• The Leapfrog Group President and CEO Leah Binder recently appeared on the Business Group on Health podcast to discuss transparency around hospital quality and safety. She shared how hospitals can use quality and safety data to improve their processes and how both employers and consumers can use it to make informed choices.
New ACAC members: United States of Care CEO Natalie Davis & the Academy of Nutrition and Dietetics
Read more: The LAN welcomes United States of Care to the Accountable Care Action Collaborative – Health Care Payment Learning & Action Network (hcp-lan.org) and The LAN welcomes new Accountable Care Action Collaborative member the Academy of Nutrition and Dietetics – Health Care Payment Learning & Action Network (hcp-lan.org)• In February, HCPLAN welcomed two new members to the ACAC. Natalie Davis, CEO of United States of Care, and the Academy of Nutrition and Dietetics both joined the ACAC to help achieve its goal of transforming the accountable care landscape. Davis’s extensive health care leadership experience and commitment to catalyze change and the Academy of Nutrition and Dietetics’ work to ensure equitable access to nutrition services will be influential assets to HCPLAN.
CMS Innovation Center Deputy Administrator and Director Liz Fowler explains new behavioral health model
Read more: CMS unveils new behavioral health model using a ‘no wrong door’ approach (fiercehealthcare.com)• CMS announced the Innovation in Behavioral Health Model, a new approach designed to improve outcomes for adults with mental health and substance use disorders. CMS Innovation Center Deputy Administrator and Director Liz Fowler provided a distinction between this model and other behavioral health models. “What differentiates this model from others is the approach. Typically, behavioral health is shoehorned into primary care settings. Since this is a community-based effort, the model calls for ‘weaving’ physical health needs into behavioral health organizations.”
Press Play: HCPLAN Executive Forum Co-Chair and Duke-Margolis Institute for Health Policy Director Dr. Mark McClellan interviewed on Prescription for Better Access
Listen now: 2024 Policy Preview: An Interview with Dr. Mark McClellan (youtube.com)• In a recent interview, Executive Forum Co-Chair Dr. Mark McClellan shared his perspective on patients’ ability to access affordable medicine. He also discussed the challenges to and opportunities for improving public health and the emerging role of artificial intelligence in health care.
Paradigm shift toward population-based payment models
Read more: A Paradigm Shift in Healthcare Payment Models: Moving towards Population-based Payments (medriva.com)• This article highlights the shift from individual service to population-based payments and the crucial role that health information technology (IT) plays. “CMS’s Comprehensive Primary Care Plus (CPC+) model, for example, highlighted the importance of health IT in transforming primary care. The model emphasized the critical role of electronic health records (EHRs) and related health IT in providing core information management functionality for practices.”
Four most common value-based care arrangements
Read more: A Look Inside the Four Most Common Value-Based Care Arrangements (healthpayerintelligence.com)• The four most common value-based care arrangements are performance-based arrangements, bundled payment models, shared savings and risk-based contracts, and capitation models. This article explores each of these arrangements and explains how payers reimburse providers under each arrangement.
Our Vision
An American healthcare system that pays for value to the benefit of our patients and communities.
Our Mission
To accelerate the shift to value-based care in order to achieve better outcomes at lower cost.
Our Goal Statement
Accelerate the percentage of US healthcare payments tied to quality and value in each market segment through the adoption of two-sided risk alternative payment models.



















 Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models.
Emily DuHamel Brower, M.B.A., is senior vice president of clinical integration and physician services for Trinity Health. Emphasizing clinical integration and payment model transformation, Ms. Brower provides strategic direction related to the evolving accountable healthcare environment with strong results. Her team is currently accountable for $10.4B of medical expense for 1.6M lives in Medicare Accountable Care Organizations (ACOs), Medicare Advantage, and Medicaid and Commercial Alternative Payment Models. Mr. James Sinkoff is the Deputy Executive Officer and Chief Financial Officer for Sun River Health (formerly known as Hudson River HealthCare), and the Chief Executive Officer of Solutions 4 Community Health (S4CH); an MSO serving FQHCs and private physician practices.
Mr. James Sinkoff is the Deputy Executive Officer and Chief Financial Officer for Sun River Health (formerly known as Hudson River HealthCare), and the Chief Executive Officer of Solutions 4 Community Health (S4CH); an MSO serving FQHCs and private physician practices. Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System.
Victor is the Chief Medical Officer for TennCare, Tennessee’s Medicaid Agency. At TennCare, Victor leads the medical office to ensure quality and effective delivery of medical, pharmacy, and dental services to its members. He also leads TennCare’s opioid epidemic strategy, social determinants of health, and practice transformation initiatives across the agency. Prior to joining TennCare, Victor worked at Evolent Health supporting value-based population health care delivery. In 2013, Victor served as a White House Fellow to the Secretary of Health and Human Services. Victor completed his Internal Medicine Residency at Emory University still practices clinically as an internist in the Veteran’s Affairs Health System. Dr. Brandon G. Wilson, DrPH, MHA (he, him, his) joined Community Catalyst as the Director of the Center for Consumer Engagement in Health Innovation, where he leads the Center in bringing the community’s experience to the forefront of health systems transformation and health reform efforts, in order to deliver better care, better value and better health for every community, particularly vulnerable and historically underserved populations. The Center works directly with community advocates around the country to increase the skills and power they have to establish an effective voice at all levels of the health care system. The Center collaborates with innovative health plans, hospitals and providers to incorporate communities and their lived experience into the design of systems of care. The Center also works with state and federal policymakers to spur change that makes the health system more responsive to communities. And it provides consulting services to health plans, provider groups and other health care organizations to help them create meaningful structures for engagement with their communities.
Dr. Brandon G. Wilson, DrPH, MHA (he, him, his) joined Community Catalyst as the Director of the Center for Consumer Engagement in Health Innovation, where he leads the Center in bringing the community’s experience to the forefront of health systems transformation and health reform efforts, in order to deliver better care, better value and better health for every community, particularly vulnerable and historically underserved populations. The Center works directly with community advocates around the country to increase the skills and power they have to establish an effective voice at all levels of the health care system. The Center collaborates with innovative health plans, hospitals and providers to incorporate communities and their lived experience into the design of systems of care. The Center also works with state and federal policymakers to spur change that makes the health system more responsive to communities. And it provides consulting services to health plans, provider groups and other health care organizations to help them create meaningful structures for engagement with their communities. Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.
Tamara Ward is the SVP of Insurance Business Operations at Oscar Health, where she leads the National Network Contracting Strategy and Market Expansion & Readiness. Prior to Oscar she served as VP of Managed Care & Network Operations at TriHealth in Southwest Ohio. With over 15 years of progressive health care experience, she has been instrumental driving collaborative payer provider strategies, improving insurance operations, and building high value networks through her various roles with UHC and other large provider health systems. Her breadth and depth of experience and interest-based approach has allowed her to have success solving some of the most complex issues our industry faces today. Tam is passionate about driving change for marginalized communities, developing Oscar’s Culturally Competent Care Program- reducing healthcare disparities and improving access for the underserved population. Tamara holds a B.A. from the University of Cincinnati’s and M.B.A from Miami University.


 Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.
Dr. Peter Walsh joined the Colorado Department of Health Care Policy and Financing as the Chief Medical Officer on December 1, 2020. Prior to joining HCPF, Dr. Walsh served as a Hospital Field Representative/Surveyor at the Joint Commission, headquartered in Oakbrook Terrace, Illinois.








